The complex pattern of ‘chatter’ between different areas of an individual’s brain while they are awake could help doctors better track and even predict their response to general anaesthesia – and better identify the amount of anaesthetic necessary – according to new research from the University of Cambridge.
The complex pattern of ‘chatter’ between different areas of an individual’s brain while they are awake could help doctors better track and even predict their response to general anaesthesia – and better identify the amount of anaesthetic necessary – according to new research from the University of Cambridge.
A very good way of predicting how an individual responds to our anaesthetic was the state of their brain network activity at the start of the procedure
Srivas Chennu
Currently, patients due to undergo surgery are given a dose of anaesthetic based on the so-called ‘Marsh model’, which uses factors such as an individual’s body weight to predict the amount of drug needed. As patients ‘go under’, their levels of awareness are monitored in a relatively crude way. If they are still deemed awake, they are simply given more anaesthetic. However, general anaesthetics can carry risks, particularly if an individual has an underlying health condition such as a heart disorder.
As areas of the brain communicate with each other, they give off tell-tale signals that can give an indication of how conscious an individual is. These ‘networks’ of brain activity can be measured using an EEG (electroencephalogram), which measures electric signals as brain cells talk to each other. Cambridge researchers have previously shown that these network signatures can even be seen in some people in a vegetative state and may help doctors identify patients who are aware despite being unable to communicate. These findings build upon advances in the science of networks to tackle the challenge of understanding and measuring human consciousness.
In a study published today in the open access journal PLOS Computational Biology, funded by the Wellcome Trust, the researchers studied how these signals changed in healthy volunteers as they received an infusion of propofol, a commonly used anaesthetic.
Twenty individuals (9 male, 11 female) received a steadily increasing dose of propofol – all up to the same limit – while undergoing a task that involved pressing one button if they heard a ‘ping’ and a different button if they heard a ‘pong’. At the same time, the researchers tracked their brain network activity using an EEG.
By the time the subjects had reached the maximum dose, some individuals were still awake and able to carry out the task, while others were unconscious. As the researchers analysed the EEG readings, they found clear differences between those who were responding to the anaesthetic and those who remained able to carry on with the task. This ‘brain signature’ was evident in the network of communications between brain areas carried by alpha waves (brain cell oscillations in the frequency range of 7.5–12.5 Hz), the normal range of electrical activity of the brain when conscious and relaxed.
In fact, when the researchers looked at the baseline EEG readings before any drug was given, they already saw differences between those who would later succumb to the drug and those who were less responsive to its effects. Dividing the subjects into two groups based on their EEG readings – those with lots of brain network activity at baseline and those with less – the researchers were able to predict who would be more responsive to the drug and who would be less.
The researchers also measured levels of propofol in the blood to see if this could be used as a measure of how conscious an individual was. Although they found little correlation with the alpha wave readings in general, they did find a correlation with a specific form of brain network activity known as delta-alpha coupling. This may be able to provide a useful, non-invasive measure of the level of drug in the blood.
“A very good way of predicting how an individual responds to our anaesthetic was the state of their brain network activity at the start of the procedure,” says Dr Srivas Chennu from the Department of Clinical Neurosciences, University of Cambridge. “The greater the network activity at the start, the more anaesthetic they are likely to need to put them under.”
Dr Tristan Bekinschtein, senior author from the Department of Psychology, adds: “EEG machines are commonplace in hospitals and relatively inexpensive. With some engineering and further testing, we expect they could be adapted to help doctors optimise the amount of drug an individual needs to receive to become unconscious without increasing their risk of complications.”
Srivas Chennu will be speaking at the Cambridge Science Festival on Wednesday 16 March. During the event, ‘Brain, body and mind: new directions in the neuroscience and philosophy of consciousness’, he will be examining what it means to be conscious.
Reference
Chennu, S et al. Brain connectivity dissociates responsiveness from drug exposure during propofol induced transitions of consciousness. PLOS Computational Biology; 14 Jan 2016
Image
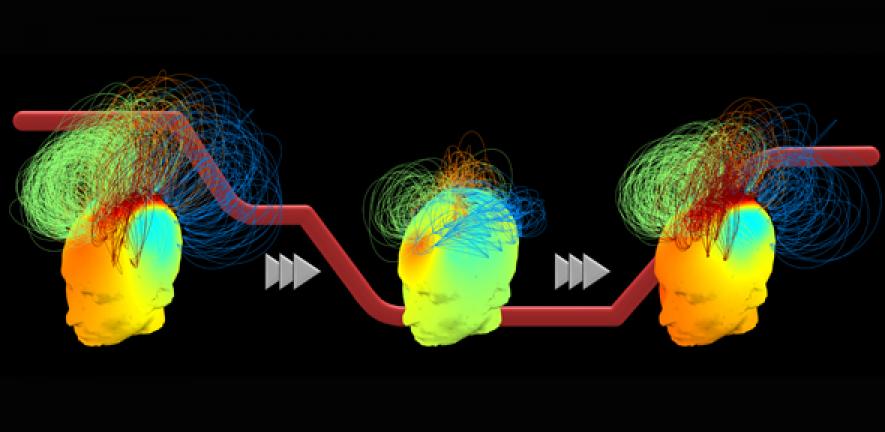
Brain networks during the transition to unconsciousness during propofol sedation (drug infusion timeline shown in red). Participants with robust networks at baseline (left panel) remained resistant to the sedative, while others showed characteristically different, weaker networks during unconsciousness (middle). All participants regained similar networks when the sedative wore off (right).

The text in this work is licensed under a Creative Commons Attribution 4.0 International License. For image use please see separate credits above.