The path from innovation to impact can be long and complex. Here we describe the 30-year journey behind the development of a drug now being used to treat multiple sclerosis.
The path from innovation to impact can be long and complex. Here we describe the 30-year journey behind the development of a drug now being used to treat multiple sclerosis.
As in other diseases, the development of Campath-1H for the treatment of MS has relied on academic researchers willing to do the basic research needed to understand how Campath-1H is working in patients and how to make it more effective.
The journey taken by Campath-1H from the laboratory to its imminent use as a new treatment for multiple sclerosis (MS) is deeply rooted in fundamental research and illustrates the role that academic research plays throughout the development of new innovations. In the late 1970s, Professor Herman Waldmann, then a lecturer in the Department of Pathology at the University of Cambridge and now Head of the Sir William Dunn School of Pathology, Oxford, was applying for his first Medical Research Council programme grant. ‘I was interested in understanding immunological tolerance [see Glossary below],’ remembers Waldmann, a process that was poorly understood at that time, as were many other aspects of the human immune system.
The immune system is a network of many cell types that protect the body from bacteria and other disease-causing organisms (pathogens). When a pathogen enters the body and infects human cells, immune system cells that circulate in the blood called T and B lymphocytes detect its presence by binding to pathogen-specific molecules called antigens and become activated. The activated T lymphocytes kill the pathogen-infected cells directly or help the activated B lymphocytes make antibodies, secreted proteins that recognise specific antigens. These antibodies coat the pathogens, which labels them for destruction by other immune system cells through processes that immunologists call effector mechanisms.
Although a person’s immune system responds quickly to pathogens, it usually ignores self antigens, molecules that are present in the person’s own body. This lack of response is called tolerance. In 1978, says Waldmann, ‘people thought that to make a good immune response, lymphocytes had to cooperate with each other and that if there wasn’t good cooperation between lymphocytes, the default state was tolerance.’
One way to investigate tolerance, therefore, might be to reduce the number of lymphocytes in an experimental animal and then expose the animal to a new antigen. If this theory about tolerance was right, the animal should become tolerant to the antigen. But how could the number of lymphocytes in an animal be reduced?
The approach Waldmann took was to make an anti-lymphocyte antibody using a technique that had recently been developed by Dr César Milstein at the nearby Laboratory of Molecular Biology. By fusing myeloma cells (cancer cells that develop from B lymphocytes) with cells from the spleen, Milstein had managed to make cell lines that indefinitely produced large amounts of a single antibody. Such monoclonal antibodies were ideal for Waldmann’s experiment.
‘The immediate medical applications of this experiment were very clear,’ says Waldmann. ‘If it worked, it would provide a way to improve bone marrow transplants.’ These transplants are used to ‘rescue’ cancer patients whose blood system has been destroyed by radiotherapy. Donated bone marrow rescues these patients because it contains stem cells, precursor cells that can provide the recipient with a new blood system. Unfortunately, donated bone marrow also contains mature lymphocytes, which can attack the patient. Waldmann reasoned that, by using a monoclonal antibody to remove mature lymphocytes from the donor marrow, this potentially fatal ‘graft-versus-host disease’ could be avoided. Importantly, however, Waldmann also saw his work as a way to investigate basic immunological mechanisms.
Campath antibodies and bone marrow transplants
Late in 1979, Waldmann and his team immunised a rat with human lymphocytes and fused its spleen cells with a rat myeloma cell line. Over Christmas, Waldmann isolated several antibody-producing cell lines from this Campath-1 fusion (‘Campath’ stands for Cambridge Pathology) and his team set to work to identify an antibody that could kill mature T lymphocytes without damaging the bone marrow stem cells. In particular, the researchers looked for an antibody that could activate complement, one of the immune system’s effector mechanisms. The monoclonal antibody that best met these criteria was an ‘IgM’ antibody. B lymphocytes can make several different types of antibody (isotypes), each of which behaves differently in terms of which immune effector mechanisms it interacts with to destroy pathogens. This particular IgM (Campath-1M) activated complement efficiently and almost completely eliminated T lymphocytes in test tubes.
The first bone marrow transplants that used Campath-1M for T-lymphocyte depletion were performed in the early 1980s. Bone marrow taken from donors was treated with Campath-1M in test tubes and the T-lymphocyte-depleted bone marrow was then injected into the graft recipients. This procedure successfully reduced the incidence of graft-versus-host disease but a new problem soon became evident. Some of the bone marrow recipients rejected the transplant. Their immune system had recognised the marrow as foreign even though the patients had been given drugs before the transplant to suppress their immune responses. Clearly, a better method was needed to suppress the patient’s immune response.
An obvious way to do this was to treat both the donor bone marrow and the transplant recipient with a T-lymphocyte-depleting antibody but the researchers knew that Campath-1M worked poorly in patients so they returned to the laboratory to find another antibody isotype that would be more effective. Their results suggested that an IgG2b antibody was likely to work best. Unfortunately, none of the antibodies produced in the Campath-1 fusion had this isotype. However, monoclonal-antibody-producing cell lines sometimes spontaneously start to make antibodies of a different isotype. So, the researchers painstakingly screened a cell line that was making an IgG2a antibody until they found a cell that had switched to making an IgG2b antibody – Campath-1G. Like the original Campath-1M (and Campath-1H; see below), Campath-1G binds to a molecule called CD52 that is present on lymphocytes and some other human cells.
Campath-1G and Campath-1H go into patients
‘Once we knew we had an antibody that worked in patients, we started to talk to a variety of clinicians who might be interested in using an anti-lymphocyte antibody,’ explains Waldmann. Some of these clinicians were treating patients who had lymphocytic leukaemia, a blood cancer in which lymphocytes replicate uncontrollably. Two patients with this type of cancer were duly treated with Campath-1G and initially responded well although both patients subsequently relapsed. In one patient, their immune system had recognised Campath-1G – a rat antibody – as foreign and destroyed it.
Clearly, a more-nearly human antibody was needed that would be ignored by the human immune system. Fortuitously, another Cambridge scientist, Professor Sir Greg Winter, had just developed a way to ‘humanise’ antibodies. Humanisation is the replacement of some regions in an animal antibody by the equivalent human regions; the animal regions that determine which antigen the antibody recognises are retained in humanised antibodies. Dr Mike Clark, who had joined Waldmann’s laboratory in 1981, started to make a set of fully and partly humanised antibodies from Campath-1G and, together with other team members, tried to determine which human isotypes would work in patients. Campath-1H, a humanised IgG1, was the result of all this basic research although, says Clark, who is now a Reader in Therapeutic Immunology in the Department of Pathology, University of Cambridge, ‘these days, we think that a partly humanised antibody that retained some more of the rat regions would probably have worked just as well.’
Campath-1H was very successful for the treatment of lymphocytic leukaemia and of non-Hodgkin lymphoma (another type of blood cancer), and for use in bone marrow and solid organ transplants. Clinicians also started to use it to treat several autoimmune diseases including vasculitis (inflammation of the blood vessels), rheumatoid arthritis and MS. The clinical-grade material needed for these studies was produced in the Therapeutic Antibody Centre (TAC) that Waldmann set up in Cambridge in 1990 with Professor Geoff Hale, a biochemist who had joined Waldmann’s group at the beginning of the Campath-1H story and who is now Visiting Professor of Therapeutic Immunology at the Sir William Dunn School of Pathology, Oxford. The TAC moved to Oxford in 1995. ‘Without Geoff’s critical contribution and the support of both Cambridge and Oxford University,’ says Waldmann, ‘we would not have been able to initiate many of these studies, including our long-standing collaboration with Alastair Compston in MS.’
Pharmaceutical company involvement
The development of a drug for clinical use is a highly regulated, long and expensive process, so drugs only get to market if pharmaceutical companies become involved in their development. In the early 1980s, the Cambridge researchers assigned the rights for the Campath-1 cell lines to BTG, originally a government body set up to facilitate the exploitation of inventions from UK academics but now an international specialty pharmaceuticals company. In 1985, BTG licensed Campath-1M to Wellcome Biotech, a subsidiary of the Wellcome Foundation. ‘Many people were very sceptical in the mid-1980s about the commercial future of antibodies and other biotech drugs but Wellcome was excited by the potential of this new area,’ comments Dr Richard Jennings (Director of Technology Transfer and Consultancy Services, Cambridge Enterprise Ltd).
When the basic research being undertaken by Waldmann’s team suggested that Campath-1G and Campath-1H were more likely to have a clinical future than Campath-1M, these antibodies were also licensed to Wellcome Biotech. Indeed, once Campath-1H had been handed over, the company abandoned its work on the earlier antibodies and started a programme of clinical trials of Campath-1H in rheumatoid arthritis, leukaemia and lymphoma. Meanwhile, the academic scientists continued with their basic research, refining and extending their understanding of how Campath-1H was working in various diseases by collaborating closely with the physicians who were giving the antibody to patients. This research was helped along by the development of new molecular techniques and by improved understanding of the human immune system.
Then, in 1995, Wellcome (which merged with Glaxo that year to become Glaxo-Wellcome) decided to abandon its development of Campath-1H, fearing that Campath-1H would not have a billion-dollar market after all. Although the antibody worked well in some types of leukaemia, it did not work in all leukaemias and, in the rheumatoid arthritis trials, Campath-1H had permanently suppressed patients’ immune systems. This decision was very disappointing for Waldmann and his colleagues, who strongly believed in the clinical potential of Campath-1H. ‘We looked at things from a different point of view,’ says Waldmann. ‘As academic scientists, when Campath-1H caused unexpected side effects or did not work as well as expected, our response was to look at the evidence, figure out what had gone wrong, and find ways to put it right rather than giving up.’
In 1997, after protracted negotiations with BTG and Glaxo-Wellcome, LeukoSite Inc. took on the licence to develop Campath-1H. LeukoSite, which merged with Millennium Pharmaceuticals in 1999, partnered with ILEX Oncology to complete the development and obtain US approval in 2001 for Campath-1H to be used for the treatment of B-cell chronic lymphocytic leukaemia (CLL) in patients who had failed to respond to conventional chemotherapy. The licence for Campath-1H was then transferred to ILEX Oncology before, finally, in 2004, Genzyme Corporation acquired ILEX Oncology and the production rights to Campath-1H.
Says Mark Enyedy, Senior Vice- President at Genzyme, ‘Campath-1H has had a particularly tortuous commercial history. I think the many changes of commercial support for this product have impeded the realisation of this drug’s commercial potential even though products like this always take an enormous time to develop.’
MS – Campath-1H’s new market?
Last year, the revenue from the use of Campath-1H for the treatment of CLL was around US$100 million but this income may eventually be dwarfed by the revenue generated from the treatment of early relapsing–remitting MS with Campath-1H (the generic name for the drug is alemtuzumab; its registered name is Campath®). As in other diseases, the development of Campath-1H for the treatment of MS has relied on academic researchers willing to do the basic research needed to understand how Campath-1H is working in patients and how to make it more effective.
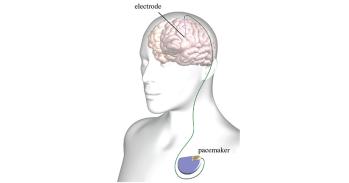
MS is an inflammatory neurological disease that is caused by damage to myelin, a substance that forms an insulating sheath around the nerve fibres in the central nervous system (CNS; the brain and spinal cord). Electrical messages pass along these nerve fibres to control conscious and unconscious actions. If the myelin sheath is damaged these messages can no longer pass smoothly and quickly between the brain and the body.
Most people with MS are initially diagnosed with relapsing–remitting MS. In this form of the disease, symptoms (which include muscle spasms and stiffness, tremors, bladder and bowel control problems, and pain) occur in episodes that are followed by periods of spontaneous recovery (remissions). Relapses can occur at any time, last for days, weeks or months, and vary in their severity. Most people who have relapsing–remitting MS eventually develop secondary progressive MS in which the occurrence of relapses wanes but overall disability slowly increases.
Early attempts to treat MS
By the late 1980s, it was becoming clear that MS is an autoimmune disease (a disease in which a person’s immune system attacks the person’s own tissues) in which activated T lymphocytes move into the CNS and damage myelin. As Professor Alastair Compston (Professor of Neurology and Head of the Department of Clinical Neurosciences at the University of Cambridge) explains, ‘we began to wonder whether we could help patients with MS by preventing the movement of activated lymphocytes from the bloodstream into the brain.’ Treatment with Campath-1H looked like one way that this could be achieved and, in 1991, Compston started an 18-year-long collaboration with Waldmann and his team by trying this approach for the first time in a woman who had developed MS some years earlier. ‘At that time, there were no licensed treatments for MS,’ says Compston, ‘and this individual seemed to be facing a particularly grim future. Alarmingly, she actually got much worse for a day or two after receiving Campath-1H but then picked up and remained very well for some years. She even seemed to get back some of her lost functions.’
Keeping in close contact with Waldmann’s team, Compston and colleagues carefully followed the progress of their patient for about 18 months before treating another six people. ‘By 1994, we had satisfied ourselves that Campath-1H treatment could stop the development of new inflammatory lesions in the brain,’ says Compston. In addition, ‘it seemed as though our patients had fewer new attacks after the treatment.’
By 1999, Compston and a clinical trainee, Dr Alasdair Coles, had treated 27 patients, all of whom had already entered the secondary progressive stage of MS. ‘We paused then to analyse our results,’ says Compston. &lsq
uo;We realised that, although we had stopped disease activity in terms of new inflammatory brain lesions and had reduced the number of attacks that people were having, most of our patients were continuing to deteriorate.’ The problems that the patients had had when they started Campath-1H treatment were slowly progressing. This observation puzzled the researchers. If MS is an inflammatory autoimmune disease, why was Campath-1H treatment failing to help people in the progressive phase of the disease even though the treatment seemed to turn off inflammation?
The answer to this conundrum, the researchers realised, is that there are two separate processes going on in MS – inflammation and degeneration. Inflammation causes the attacks in relapsing–remitting MS but also triggers nerve degeneration. Eventually, the degenerative component of the disease gains a momentum of its own and continues even in the absence of inflammation, which results in slow progression and the accumulation of disabilities that don’t get better. ‘Until we used Campath-1H in patients, this separation between inflammation and degeneration was not appreciated,’ says Compston, ‘but its implications were obvious. If this drug was going to be of any use to people with MS, we would have to use it much earlier in the disease process than we had so far.’
Campath-1H for the treatment of relapsing–remitting MS
Compston and Coles now began to treat some of their patients with relapsing–remitting MS with Campath-1H. As before, the treatment almost completely stopped new attacks occurring but, in addition, many of these patients actually began to get better. Their various disabilities began to improve. It was time to take Campath-1H into formal clinical trials to prove the drug’s efficacy and to prepare the way for marketing the drug for the treatment of MS.
With the support of ILEX Oncology (and, from 2004, of Genzyme), a Phase 2 clinical trial was started in December 2002. Patients enrolled into the trial had to meet strict entry criteria and were treated with up to three annual doses of Campath-1H. The effects of the drug were measured three years after the initial treatment and, unusually for a Phase 2 trial, its effects were compared with the effects of another drug – interferon beta-1a, the current gold standard treatment for MS. ‘We set the bar high in this trial,’ says Enyedy. ‘Most studies of treatments for MS compare the new treatment with a placebo and only last a year.’ Genzyme, adds Compston, ‘has been fantastically committed to the development of Campath-1H for use in MS.’
The results of the trial, which were published in 2008 in theNew England Journal of Medicine, showed that there were 70% fewer relapses and that the risk of accumulated disability was 70% lower among the patients receiving Campath-1H than among those treated with interferon beta-1a. Furthermore, as in the patients treated before the trial started, the disability score of patients treated with Campath-1H actually improved; by contrast, it worsened in the patients given interferon beta-1a.
Two large Phase 3 trials are now under way that will finish in 2011. If all goes well, Genzyme expects to apply for marketing approval in 2012, 21 years after the first patient with MS was treated with Campath-1H (and 33 years after Waldmann’s team started the research that produced Campath-1H). ‘So far, ‘ says Compston, ‘we have spent 18 years carefully observing treated patients and learning from our mistakes… With more secure funding for our basic and clinical research in the 1990s, we might have been able to move more quickly. But with a disease like MS, which was then poorly understood, it was always going to take a long while to develop a new drug.’ Importantly, adds Enyedy, ‘if the Phase 3 trials are successful, I think we can stake a claim for a new standard of care for a large subset of patients with relapsing–remitting MS,’ a prospect that, Compston says, is ‘very rewarding for a clinical neurologist who has seen so many young people lose the ability to perform simple aspects of everyday living as a result of this difficult disease.’
Glossary
Antibody: a secreted protein made by the immune system that binds to a specific molecule called its antigen. Antibody binding to an antigen on the surface of pathogens (disease-causing organisms) recruits other parts of the immune system to kill the pathogen. Antibodies are members of a family of proteins called immunoglobulins (Ig).
Antigen: any molecule that can bind specifically to an antibody.
Autoimmune disease: a disease in which the immune system mounts a response against self antigens.
B lymphocyte: a type of white blood cell that makes antibodies.
Bone marrow: the spongy material inside bones where all the cells in the blood, including red blood cells and lymphocytes, are made.
Complement: a set of blood proteins that form one of the immune system’s mechanisms for killing pathogens.
Isotypes: different classes of immunoglobulins such as IgG and IgM. Some of the isotypes have subclasses. For example, there are four human IgG subclasses – IgG1, IgG2, IgG3 and IgG4.
Monoclonal antibodies: antibodies that are made artificially in the laboratory.
Self antigens: molecules that are in an individual’s own tissues.
T lymphocytes: a type of white blood cell that helps B lymphocytes make antibodies and that also directly kills pathogen-infected cells.
Tolerance: the failure to respond to an antigen. The immune system is usually tolerant to self antigens.
A tale of two innovations
We are often taken aback by the sudden appearance of a new innovation that has clear economic or clinical impact. Just how did these innovations arise?
Academic scientists working in universities are driven to do their research for many reasons. Some see their research as a way to develop new drugs or to build more powerful computers, for example. Many academic scientists, however, are simply curious about the world around them. They may want to understand the intricacies of the immune system or how the physical structure of a material determines its properties at a purely intellectual level. They may never intend to make any practical use of the knowledge that they glean from their studies.
Importantly, however, even the most basic, most fundamental research can be the starting point for the development of materials and technologies that make a real difference to the everyday life of ordinary people and that bring economic benefit to the country. Indeed, said Dr Richard Jennings, Director of Technology Transfer and Consultancy Services at Cambridge Enterprise Ltd, University of Cambridge, ‘what universities are good at is fundamental research and it is high-quality basic research that generates the really exciting ideas that are going to change the world.’
But it takes a great deal of time, money and commitment to progress from a piece of basic research to a commercial product, and the complex journey from the laboratory to the marketplace can succeed only if there is long-term governmental support for the academic scientists and their ideas as well as the involvement of committed commercial partners and well-funded technology transfer offices.
Two particular stories illustrate the long and complex path taken from the laboratory to commercial success by two very different University of Cambridge innovations. In the case of Plastic Logic, basic research on materials called organic semiconductors that started in the 1980s and that continues today has led to the development of a new type of electronic reader that should be marketed in early 2010 and, more generally, to the development of ‘plastic electronics’, a radical innovation that could eventually parallel silicon-based electronics. For Campath, the journey started just before Christmas in 1979 in a laboratory where researchers were trying to understand an immunological concept called tolerance. Now, nearly three decades later and after a considerable amount of both basic research and commercial development, Campath-1H is in Phase 3 clinical trials for the treatment of relapsing–remitting multiple sclerosis.
‘Both innovations are likely to have profound impacts over the next two years and it is important to recognise the deep temporal roots of both,’ said Professor Ian Leslie, Pro-Vice-Chancellor for Research.
Professor Leslie highlighted that an important lesson to draw from these stories ‘is the need for universities and other recipients of public research funding to implement and develop processes to support the translation of discovery to impact or, more generally, to develop environments in which the results of discovery can be taken forward and in which external opportunities for innovation are understood.’
This work is licensed under a Creative Commons Licence. If you use this content on your site please link back to this page.