Researchers have identified how the ‘wall’ around cancer tumours functions and how to break it down, enabling the body’s own defences to reach and kill the cancer cells within.
Researchers have identified how the ‘wall’ around cancer tumours functions and how to break it down, enabling the body’s own defences to reach and kill the cancer cells within.
By enabling the body to use its own defences to attack cancer, this approach has the potential to greatly improve treatment of solid tumours
Doug Fearon
A possible new method for treating pancreatic cancer which enables the body’s immune system to attack and kill cancer cells has been developed by researchers.
The method uses a drug which breaks down the protective barrier surrounding pancreatic cancer tumours, enabling cancer-attacking T cells to get through. The drug is used in combination with an antibody that blocks a second target, which improves the activity of these T cells.
Initial tests of the combined treatment, carried out in mice by researchers at the University’s Cancer Research UK Cambridge Institute, resulted in almost complete elimination of cancer cells in one week. The findings, reported in the journal PNAS, mark the first time this has been achieved in any pancreatic cancer animal model. In addition to pancreatic cancer, the approach could potentially be used in other types of solid tumour cancers.
Pancreatic cancer is the fifth most common cause of cancer-related death in the UK and the eighth most common worldwide. It affects men and women equally, and is more common in people over the age of 60.
As it has very few symptoms in its early stages, pancreatic cancer is usually only diagnosed once it is relatively advanced, and prognosis is poor: for all stages combined, the one and five-year survival rates are less than 20% and less than 4% respectively. Tumour removal is the most effective treatment, but it is suitable for just one in five patients.
Immunotherapy – stimulating the immune system to attack cancer cells – is a promising therapy for several types of solid tumours, but patients with pancreatic cancer have not responded to this approach, perhaps because the human form of the cancer, as in animal models, also creates a protective barrier around itself.
The research, led by Professor Douglas Fearon, determined that this barrier is created by a chemokine protein, CXCL12, which is produced by a specialised kind of connective tissue cell, called a carcinoma-associated fibroblast, or CAF. The CXCL12 protein then coats the cancer cells where it acts as a biological shield that keeps T cells away. The effect of the shield was overcome by using a drug that specifically prevents the T cells from interacting with CXCL12.
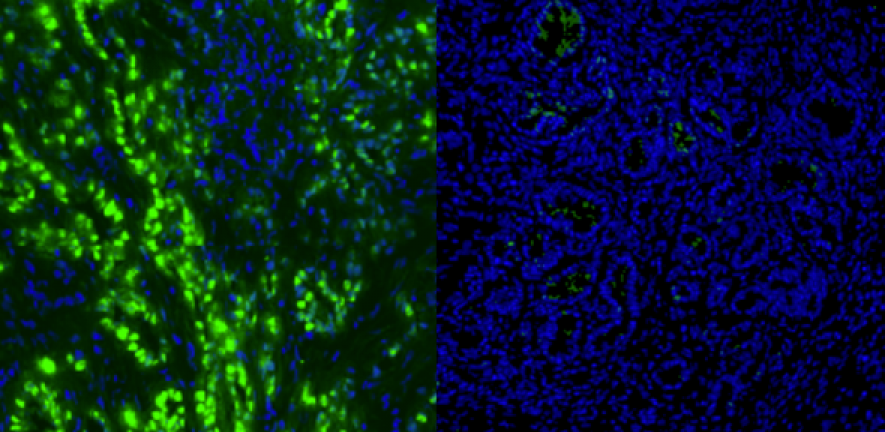
“We observed that T cells were absent from the part of the tumour containing the cancer cells that were coated with chemokine, and the principal source of the chemokine was the CAFs,” said Professor Fearon. “Interestingly, depleting the CAFs from the pancreatic cancer had a similar effect of allowing immune control of the tumour growth.”
The drug used by the researchers was AMD3100, also known as Plerixafor, which blocks CXCR4, the receptor on the T cells for CXCL12, enabling T cells to reach and kill the cancer cells in pancreatic cancer models. When used in combination with anti-PD-L1, an immunotherapeutic antibody which enhances the activation of the T cells, the number of cancer cells and the volume of the tumour were greatly diminished. Following combined treatment for one week, the residual tumour was composed only of premalignant cells and inflammatory cells.
“By enabling the body to use its own defences to attack cancer, this approach has the potential to greatly improve treatment of solid tumours,” said Professor Fearon.
The research was supported by GlaxoSmithKline, the Medical Research Council, Addenbrooke’s Charitable Trust, the Ludwig Institute for Cancer Research, the Anthony Cerami and Anne Dunne Foundation for World Health, and Cancer Research UK.
For more information, please contact Sarah Collins on sarah.collins@admin.cam.ac.uk.
This work is licensed under a Creative Commons Licence. If you use this content on your site please link back to this page.