Surviving birth

Researchers at one of the busiest maternity hospitals in the world aim to help more women survive complications giving birth.
Obstetrician Dr Annettee Nakimuli and colleagues look after up to 28,000 births a year at Mulago Hospital in Kampala, Uganda.
Every day, 300 pregnant women visit the hospital antenatal clinic. Around 100 women are on the labour ward, and 40 of these will have complications – obstructed labour, haemorrhage, sepsis or pre-eclampsia – requiring up to 25 emergency caesarean sections to be carried out.
“When women come to the labour ward they hope to come out with the best of it – they hope to come out with a live baby, and come out alive themselves. But women go to hospital with mixed feelings – they’ve seen others die before them, so there’s a tendency to think of maternal death as something inevitable rather than avoidable,” says Nakimuli, who is also Chair of the Department of Obstetrics and Gynaecology at Makerere University in Kampala.
“In a bad month, we can have up to 15 mothers dying. For babies, the number is usually double or three times that figure.”
Part of the challenge is the sheer number of patients compared with the number of doctors and midwives.
“We are a national referral hospital so we receive everybody... we can’t deny admission because we are full,” says Nakimuli. “In fact we’re not even sure what full means – we’ve always worked above 100% capacity.”
Nevertheless, Nakimuli is convinced that, even with these difficulties, something can be done to reduce the mortality rate. Despite an astonishing workload, she and others are questioning why the level of maternal deaths is so high in sub-Saharan Africa.
IN NUMBERS...
Level of maternal deaths are nearly 50 times higher for women in sub-Saharan Africa and their babies are 10 times more likely to die in their first month of life compared with high-income countries.
Women in sub-Saharan Africa face a 1 in 37 lifetime risk of dying during pregnancy or childbirth. By comparison, the lifetime risk for a woman in Europe is 1 in 6,500.
Child and maternal mortality estimates released September 2019 by UNICEF and the World Health Organization.
Silent killer
Ten years ago, Nakimuli arrived in Cambridge as part of the Cambridge-Africa Programme, a University-wide initiative to make its expertise and resources available to support ‘African researchers working in Africa on African priorities’.
She was embarking on a PhD with Professor Ashley Moffett, an expert on the life-threatening condition pre-eclampsia that results from the placenta developing abnormally.
Pre-eclampsia occurs more commonly in women of African ancestry compared with Europeans, and happens earlier in pregnancy and is more severe, says Moffett: “What makes the disease a ‘silent killer’ is that it’s impossible to predict or prevent. The only course of action is careful monitoring and emergency delivery.”
Over the past decade, Nakimuli has travelled back and forth between her research lab at Makerere University in Kampala and Cambridge’s Department of Pathology to learn techniques, analyse samples and spend time with Moffett examining why this complex disease is so much more of a problem in Africa.
Their collaboration led to the discovery of particular genes found only in women of African descent that are linked with risk and protection in pre-eclampsia.

Professor Ashley Moffett and Dr Annettee Nakimuli (photography: Lloyd Mann)
Professor Ashley Moffett and Dr Annettee Nakimuli (photography: Lloyd Mann)
Moffett is now hopeful that recent work on ‘mini-placentas’ with Cambridge colleagues Dr Margherita Turco (see panel below) and Professor Graham Burton will provide a much-needed experimental tool to understand this mysterious disease – and the role of the placenta in general.
But even with these major steps forward, the researchers know they are still a long way off being able to offer early diagnosis and treatment, as Nakimuli explains: “I’ve really worked on trying to understand pre-eclampsia and we’ve made discoveries that will help us to understand the basic disease, but sometimes the endpoint of being able to help the patients is not easy to reach. In the meantime, it’s very obvious that we need to find other ways of helping women right now.”
Stories to books
Ugandan obstetrician Dr Imelda Namagembe is also trying to improve maternal health by, as she explains, “learning from the stories of the women who have died.”
In the UK, if a woman dies during or after pregnancy, the circumstances of her death are collected anonymously by a national service called MBRRACE (Mothers and Babies; Reducing Risks through Audits & Confidential Enquiries across the UK), which then makes national recommendations to improve future care.
Namagembe would like to see a similar system in Uganda, where the level of systematic processing and reviewing of reasons for maternal death is low.
The first step is to identify the barriers to this process, which she is doing for her PhD as part of the Cambridge-Africa Programme, co-supervised by Nakimuli and Dr Catherine Aiken from Cambridge’s Department of Obstetrics and Gynaecology.
“One of the things that makes an enormous difference to women surviving is somebody systematically collecting the reasons why mothers have died, reviewing them, understanding what’s happening, and then learning from it, and no one has done this in Uganda,” says Aiken.
She adds: “Given the pressure that doctors like Imelda and Annettee are under, it’s amazing that there’s also the will and the determination to say look we can do something about this.”
It’s a sentiment echoed by Aiken’s colleague, Dr Charlotte Patient, a Consultant Obstetrician at the Rosie Maternity Hospital in Cambridge, part of Cambridge University Hospitals NHS Foundation Trust. Patient also visits Kampala each year with a volunteer team of NHS clinicians and midwives from the Rosie organised by Cambridge Global Health Partnerships.
“The staff in Kampala don’t need clinical expertise – they’re very good,” says Patient. “What they asked us for help with was in building clinical guidelines that could be used everywhere and updated easily. They’d had no breathing space to take a step back and develop standardised approaches.”
As the Ugandan and Cambridge teams worked together to develop guidelines for the major causes of maternal mortality, there were some unexpected successes, says Nakimuli: “Our midwives gained confidence. We saw, for example, Charlotte the doctor and Kimberley the midwife discuss matters as equal partners. It showed us how interdisciplinary teams work well. Around 80% of our deliveries are in the hands of midwives, and so the more empowered they are, the better.”
Back in the UK, Patient says she has a new perspective on her own work: “You come back with a completely different appreciation for the NHS. I really think about use of resources and how we don’t always make best use of what we have. The experience has made me a better doctor.”
“Given the pressure that doctors like Imelda and Annettee are under, it’s amazing that there’s also the will and the determination to say look we can do something about this.”
Dr Catherine Aiken, Department of Obstetrics and Gynaecology
Another success is on the way to being born: the first contemporary textbook of obstetrics written by African doctors for African women. Nakimuli and her Ugandan colleagues are currently writing the contents planned for publication in print and online by Cambridge University Press in 2021. Meanwhile, her Cambridge colleagues are providing advice and have raised funds for the book to be available as open access.
Predicting outcomes
Nakimuli is also starting a new study to understand how to predict a complicated pregnancy. Her Pregnancy Outcome Prediction Study (or POPs), funded by the Royal Society and the African Academy of Sciences, and thought to be the first of its kind in Africa, is based on a model designed by Professor Gordon Smith in Cambridge’s Department of Obstetrics and Gynaecology.
Smith’s study followed 4,212 UK women for five years from early pregnancy through to delivery in order to identify predictors of adverse pregnancy outcomes.
“In the UK, although some women are identified as high risk for pregnancy complications from their medical history, most complications occur in women with no known risk factors,” he explains.
Smith’s unique data-rich approach looks for the ‘biological signature’ of an unhealthy pregnancy using regular ultrasound scans and blood sampling, DNA sequencing, analysis of samples of placenta, fetal membranes and umbilical cord, and details of the delivery and outcome.
The huge volume of data is already providing health benefits: for instance, his team discovered that offering universal late pregnancy ultrasounds at 36 weeks’ gestation eliminates undiagnosed breech presentations of babies, lowers the rate of emergency caesarean sections, improves the health of mothers and babies, and could actually save the NHS money.
“Practice only changes when guidelines change, and guidelines only change when the evidence to support change is strong,” adds Smith.

“What motivates me is the belief that I will see preventable maternal death being talked about as a thing of the past.” (Photography: Lloyd Mann)
“What motivates me is the belief that I will see preventable maternal death being talked about as a thing of the past.” (Photography: Lloyd Mann)
Nakimuli’s goal is to look specifically at the ‘signature’ for pre-eclampsia: “Until now we have been studying the women who have developed the disease,” she says. “We need to move a stage earlier and do prospective studies that will help us to understand which women we should pay special attention to when they become pregnant.
Because African women have more severe forms of the disease, we think this is an opportunity to understand the disease as never before.”
Moffett believes that Nakimuli has the passion and ability to make a difference: “She’s a leader. She’s not only established and maintained these wonderful collaborations between Makerere University and Cambridge but she’s been a role model for all the other collaborations that now exist in areas like sepsis, placental malaria, hypertension, anaesthesia and infection control.
“For change to happen it needs to be led by Africans like Annettee.”
Professor Ashley Moffett, Department of Pathology
Nakimuli herself is optimistic that the small successes in reducing the rate of maternal mortality in Africa will become bigger successes: “Globally, maternal and neonatal health has become a high priority among the international community, and there is more awareness in Africa that we should not accept that it is normal to die during childbirth. We are seeing small successes so, when they announce every few years there is a bit of decline, I think: yes… we will finally get there.
“What motivates me every day is the belief that, in my lifetime, I will see preventable maternal death being talked about as a thing of the past, even within sub-Saharan Africa.”
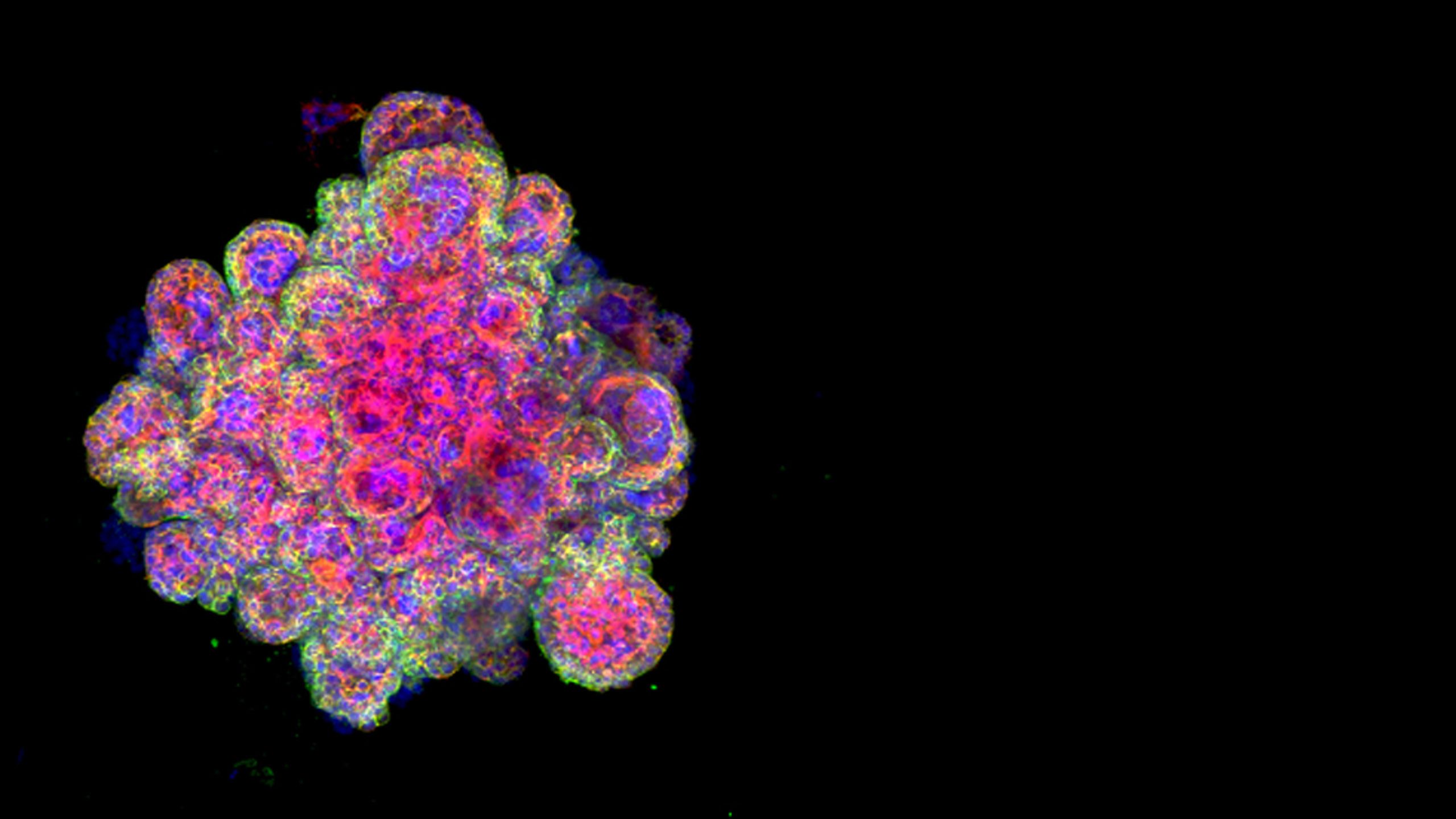
Snapshot: The placenta grower
Pregnancy complications are often the result of defective placental development and function. But how and why this should happen is a ‘black box’. These are particularly human problems and it’s not possible to study the organ inside the mother.
So Dr Margherita Turco working with Professors Ashley Moffett and Graham Burton came up with a transformative solution: she grew a uterus and a placenta in a dish. “Without a reliable experimental model that mimics how placental cells interact with the maternal tissues, it was impossible to ask even basic questions,” says Turco, from the Department of Pathology and Centre for Trophoblast Research.
“We can now grow miniature functional ‘organoids’ that so closely resemble first-trimester placentas that the cells record a positive response using a pregnancy test, showing they are secreting hormones.
“Our mini-placentas will help to shed light on the mysteries surrounding the relationships between the placenta, uterus and fetus. They could be used to understand the role of the placenta to protect the baby and how chromosomal abnormalities perturb normal development, as well as to screen the safety of drugs to be used in early pregnancy.
“To me, one of the most exciting aspects is that the events when a mother and her fetus first physically interact through the uterus and placenta have been impossible to capture. Now we can see exactly what happens when the two sides ‘talk’ to each other, and if that dialogue is perturbed in women who suffer an early pregnancy loss.”
Image: Trophoblast organoid (Margherita Turco).
Read more about our research into all aspects of reproduction in Horizons (PDF), the University of Cambridge's research magazine, and find related articles online.
Cambridge Reproduction Strategic Research Initiative
From understanding ancient ideas of generation to exploring new frontiers in fertility, Cambridge researchers are working across disciplines to study reproduction from multiple perspectives. For more information, visit the Cambridge Reproduction Strategic Research Initiative website.