Training a new breed of clinical triallist
Cambridge’s Experimental Medicine Initiative

These days, thanks to COVID, we are all aware of the importance of clinical trials in getting new treatments to patients. But only around 15% of drugs trialled are ever approved and they often fail at a very late stage, costing the pharmaceutical industry trillions of dollars.
Cambridge's Experimental Medicine Initiative (EMI), supported by AstraZeneca and GSK, is training a new kind of triallist, specialists who can work out at an early stage if a treatment is likely to succeed.
More than 20,000 talented researchers, clinicians and healthcare professionals live and work in and around Cambridge. These are people with one thing in common: a determination to find new and better ways of preventing and treating disease.
But before a new treatment can be used with patients, it has to go through exhaustive clinical trials. This is a process we have become all too familiar with, as we watched the race to develop effective COVID vaccines unfold.
“The world now knows that being able to test the effectiveness of new vaccines and other medicines in a safe and timely manner is critical both to future public health emergencies and to the development of new treatments for chronic diseases,” says Ian Wilkinson, Professor of Therapeutics and Director of the Cambridge Clinical Trials Unit.

Professor Ian Wilkinson
Professor Ian Wilkinson
Before they were so abruptly brought to public consciousness, clinical trials had been evolving over the course of the twentieth and twenty-first centuries into a complex, highly sophisticated and heavily regulated medical specialism.
“Traditionally, clinical trials have been organised to test safety first and efficacy last,” explains Wilkinson. “It’s a cautious step-by-step approach that ensures that pharma companies can satisfy regulators that the drug is safe.”
According to Wilkinson, however, this approach, while understandable, can be problematic, as development becomes increasingly expensive and more drugs are failing at a late stage.
“When that happens,” says Wilkinson, “a company may have wasted several hundred million dollars trialling a drug that was never going to work. Leaving questions of whether a drug is effective to the final stages is now too risky and expensive.”
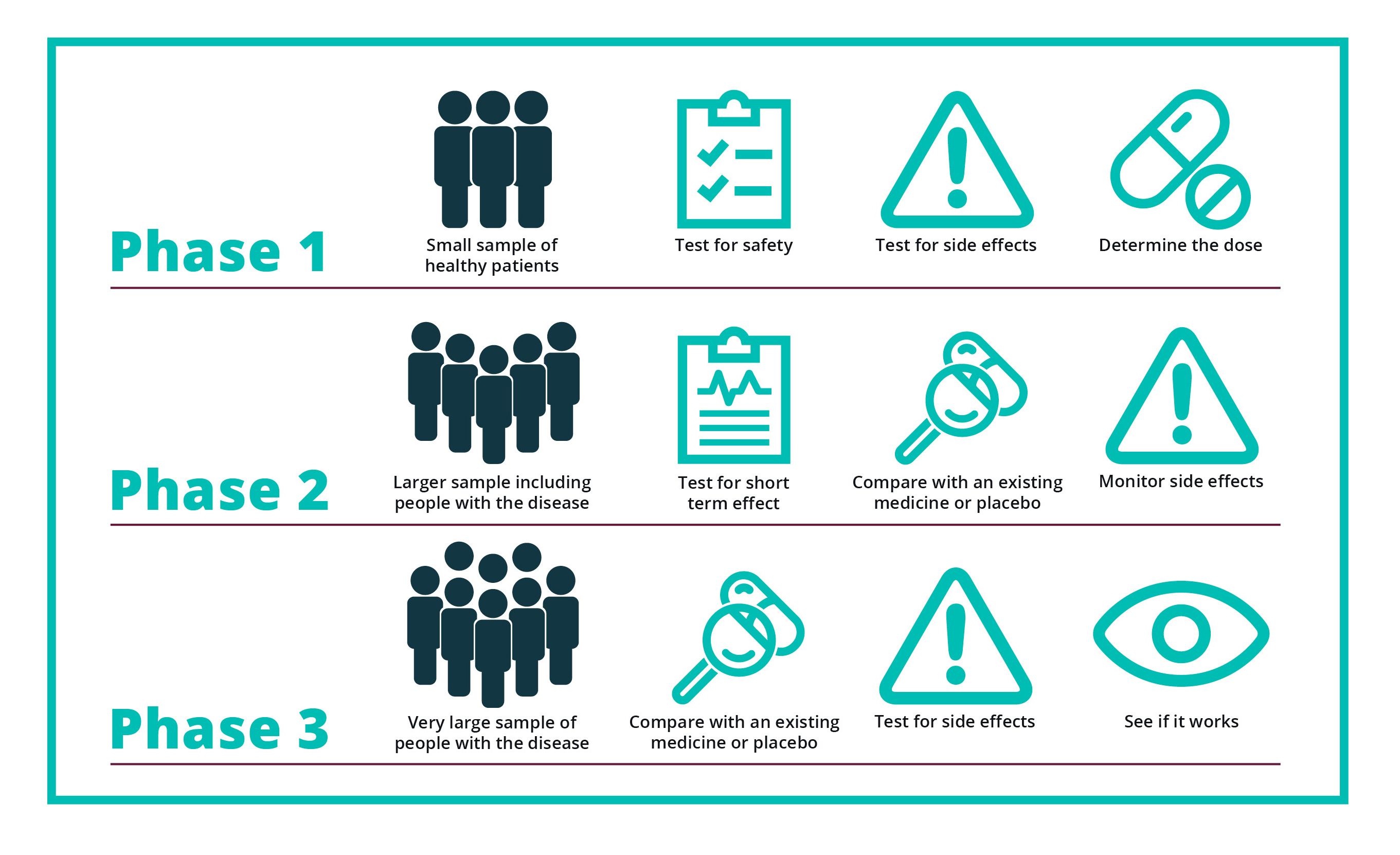
The three phases of clinical trials
The three phases of clinical trials
“We need to find out much earlier if a treatment is going to work. And we do that by looking not just at a drug’s safety in those early trials but also by studying what it’s doing to the patients. For that we need people with an unusual skillset who are in very short supply.”

A new approach
In recent years, the UK’s two pharmaceutical giants, AstraZeneca and GSK, have championed the need for more rigorous trial design to weed out likely failures earlier in the process – and have been working with the University of Cambridge to do something about it. As a collaboration, it makes perfect sense, combining the University’s research expertise with AstraZeneca and GSK’s drug discovery and development know-how.
With AstraZeneca moving its global headquarters – the Discovery Centre – to the Cambridge Biomedical Campus where GSK already has its Clinical Trials Unit, all of this expertise is now in one place, alongside not one but three, world-leading hospital trusts.
In 2016, specifically to address the shortage of suitably qualified triallists, the University set up Experimental Medicine Initiative (EMI) with funding from – and the active participation of – AstraZeneca and GSK. It has since recruited a cohort of 11 talented researchers and clinicians to its PhD programme and created six academic clinical lectureships.
The trainees all run their own clinical trials with the support of an industry, academic and clinical supervisor. The programme is designed to be a two-way street, with the trainees gaining invaluable experience while their industry partners benefit from their new approaches to experimental medicine.
"The EMI programme exemplifies how a collaboration between academia and industry supporting new clinical investigators provides clear mutual benefits.
The programme has demonstrated how innovative clinical studies using novel methodologies can inform the design of future experimental medicine studies. We have benefited from working closely with the trainees at critical times for optimising GSK clinical trials and, conversely, these interactions have enabled the trainees to experience clinical trial needs from an industry perspective."
Running a national trial to help protect vulnerable renal patients from COVID-19
Renal specialist, Dr Rona Smith was already an experienced triallist when she was appointed to an EMI academic clinical lectureship. She had previously been involved in a large international randomised trial comparing the effectiveness of drugs in patients with vasculitis, an autoimmune disease causing inflammation and narrowing of blood vessels.

Dr Rona Smith
Dr Rona Smith
From the outset, Smith was interested in asking the ‘mechanistic’ questions to “work out why some people respond to a particular drug and some don’t.”
The EMI post allowed Smith to develop her own ideas and to take on her first role as Chief Investigator in a national study, looking at responses to vaccines in vasculitis patients. In 2019, with that experience under her belt, Smith felt equipped to move on to a Senior Research Associate role.
When COVID struck, Smith and her colleague, Thomas Hiemstra, were looking after dialysis patients who, although acutely vulnerable to the virus, still had to go into hospital three times a week for treatment.
Nationally, more than 10% of dialysis patients caught COVID and those that did suffered from high mortality rates. Hiemstra had the idea that they should trial a drug that could protect both these and other vulnerable kidney patients.
Smith explains: “Speed was of the essence so we were looking to trial a drug that we already had safety data for. Various groups were busy screening drug libraries of existing compounds and the most promising appeared to be niclosamide, a drug normally used to treat tapeworms.”
The Cambridge team received enthusiastic backing from Union Therapeutics, the company that makes niclosamide, as well as funding from LifeArc, Kidney Research UK and Addenbrooke’s Charitable Trust. Getting the trial up and running was not plain sailing, however.
“The only way to get a COVID trial going in the UK was to have it designated a national priority by the government. We were turned down initially but continued to have conversations with the Department of Health. Its priority – rightly – was the vaccine roll-out but we had increasingly compelling evidence that a significant proportion of our kidney patients were still vulnerable even after two doses.”
Having agreed to modify the trial to include another nasal formulation, they eventually got the green light and have now enrolled nearly 700 patients in 36 centres across the UK. Their ambition is to reach 1,500 patients in 40 centres and the team is working with colleagues in India, with a view to extending the trial there.
Smith is excited about the trial and its prospects. “At the moment, it’s running with niclosamide, a second inhaled agent is about to be added to the platform and, moving forward, we want to refine the target population so that we can identify people who will not respond to the vaccine and therefore remain most vulnerable to the virus.
More targeted agents, such as monoclonal antibodies targeting SARS CoV-2, could also be considered for these patients.”
For Smith, her involvement in the University’s EMI programme played a pivotal role in her development as a trial specialist. “The direction of travel with all trials is to take a much more mechanistic approach, to understand why something works or doesn’t."
"Training individuals to have an understanding of the complexities of clinical trials and how to incorporate aspects of experimental medicine is key. You can only really do that by learning on the job in a supported environment. You can’t learn it remotely from textbooks. You have to be doing this kind of work to understand its intricacies.”
Treating oesophageal cancer with immunotherapy
Cancer specialist, Dr Constanza Linossi arrived in Cambridge from Argentina via Barcelona, where she had already gained first-hand experience of running clinical trials at Vall D’Hebron University Hospital, a leading international centre of clinical and translational research.
She came to Cambridge initially to work as a clinical research fellow for Addenbrooke’s Early Phase Unit and breast cancer teams. While this was valuable experience, she soon found herself “itching to design her own studies”.
Dr Constanza Linossi
Dr Constanza Linossi
To improve her knowledge of clinical trials design and gain insight in translational research, she applied to do an MPhil in translational medicine. This path took her to work at Professor Rebecca Fitzgerald’s lab, which specialises in oesophageal cancer. Although Linossi’s previous experience had been in breast and ovarian cancer, her interest quickly shifted.
“Even though it’s a nasty cancer which often has poor outcomes, oesophageal cancer has been less researched than, say, breast cancer because it is not as prevalent. ”
When Linossi heard about the EMI programme she decided to apply to further boost her experience as a translational researcher. Her EMI PhD, supported by AstraZeneca, has two separate but connected strands. Using tissue samples collected as part of a study run by Fitzgerald’s lab in collaboration with the International Cancer Genome Consortium, she is studying the molecular and immunological landscape of patients with Stage 2 and 3 oesophageal adenocarcinoma and the effects of chemotherapy on the disease. The lab work for this part of the project is carried out at AstraZeneca, under the supervision of its experts in immuno-oncology.
The design and delivery of a clinical trial, Calibration, is the second part of the project. Patients with the disease receive durvalumab, an immune checkpoint inhibitor developed by AstraZeneca. The aim of the trial is to assess its effectiveness in treating the disease and to identify biomarkers which could indicate which patients are most likely to benefit from its use.
Linossi was already an independent clinician when she arrived in Cambridge but, she says, “EMI has given me the guidance and support to set up my own early-phase trials, ask relevant research questions and help me answer them. The medical side of things is not a problem but now I have a much more complete set of skills. I can be a more critical and independent researcher."
In the future, Linossi wants to, “work in drug development at an early-phase unit of a major academic centre gaining expertise in immune-oncology - and have a really big impact on people’s lives.”
New imaging techniques for assessing the effectiveness of osteoarthritis treatments
Dr Jamie MacKay, the first of the EMI cohort to complete their PhD, was a radiologist at the Norfolk and Norwich University Hospital, who “had dabbled a bit in research” during his clinical training before deciding he wanted to pursue it further and study for a PhD.
With Fiona Gilbert, Professor of Radiology and Andrew McCaskie, Professor of Surgery at Cambridge, Mackay developed a research proposal in osteoarthritis which, it turned out, chimed with one of GSK’s strategic priorities. Interests quickly aligned and MacKay found himself enrolled in the EMI programme, working with GSK's clinicians and scientists to develop magnetic resonance imaging techniques that can be used as a rapid and non-invasive way of assessing the effectiveness of treatments for osteoarthritis of the knee. The collaboration meant that GSK could subsequently use the techniques in its experimental studies focused on osteoarthritis.
MacKay’s work has garnered international recognition. In 2020, he was elected as one of 15 Junior Fellows of the International Society for Magnetic Resonance in Medicine (ISMRM), in recognition of “outstanding quality and promise in research”. In 2021, he received the ISMRM Young investigator award for clinical MRI research, the first time the prize has been awarded outside the United States in more than 15 years.

Dr Jamie MacKay
Dr Jamie MacKay
For MacKay working with industry has opened doors: “It gave me an insight into the standards industry applies to conducting a clinical study. It was hugely beneficial to see how that world worked and definitely paved the way for me to move into my current role as a medical director in the pharmaceutical industry.”
“Our AstraZeneca R&D teams are leading the way in creating open research environments that go beyond the usual collaborative models. There are many examples where our clinicians and scientists work in collaboration with others across universities, hospitals and research institutions.
Cambridge is home to our Discovery Centre in the UK and the scale of our collaboration with others in the City is significant for our company and for patients. These external partnerships – such as the Experimental Medicine Initiative – are key to generating high impact science to support further potential advances to develop life-changing medicines for patients."
The triallists of the future
“Jamie MacKay, Coni Linossi and Rona Smith are all great examples of why the EMI programme is so important,” says Wilkinson.
“Capitalising on basic science discoveries to improve outcomes for patients is critically important and you need the right people to make it happen. That’s why the programme is vital not only to Cambridge but to the world.”
Looking ahead, Wilkinson is keen to expand the EMI, by bringing on board “more industry partners who offer more varied experiences across a wider range of disease and therapeutic areas and wider ranges of approach to therapies."
"Given that Cambridge has the greatest concentration of biopharma outside North America," he says, "it would seem that the opportunities here are fantastic both for industry and for the triallists of the future.”
The text in this work is licensed under a Creative Commons Attribution 4.0 International License.
Image at top: MarianVejcik, Getty
Infographic by Alison Fair