Inside the institute looking at early cancer
The mission of the Li Ka Shing Early Cancer Institute at Cambridge is deceptively simple: to detect cancer early enough to cure it.

The Early Cancer Institute
The Early Cancer Institute
When the Early Cancer Institute opened in 2022, it became the first physical institute in the UK dedicated to early cancer.
“Traditionally, early cancer has been neglected,” says its Director, Professor Rebecca Fitzgerald. “People have been much more focused on late cancer, advanced therapies, precision therapy, for example.”
Part of the problem is the hugely expensive and long road to get a new test or preventative treatment to market. Testing a relatively small number of patients with very advanced disease in fairly small trials is a more cost effective way of seeing if a drug works; targeting early cancer, on the other hand, would involve large population studies over several years before you know if it has worked.
“People have tended to shy away from this kind of research, but I think everyone's waking up now to the fact that unless we do this, we're not going to really improve the survival for the majority of our patients, because most patients are still diagnosed late.
"Outcomes can be completely transformed – better survival and less invasive treatments – if the cancer is diagnosed early enough, but we're just hopeless at doing that. We need to find a way to do it better.”
Professor Rebecca Fitzgerald
Researchers at the Institute are focusing in particular on cancers that are hard to treat and as such have very poor outcomes, including lung, pancreas, oesophagus and liver cancers, and acute myeloid leukaemia. Outcomes for these cancers have changed little over the past few years.
The cancers that defy treatment
Only 5% of pancreatic cancer patients survive for ten or more years
Only 10% of lung cancer patients survive for ten or more years
Only 12% of oesophageal cancer patients survive for ten or more years
Only 12% of liver cancer patients survive ten or more years
Only 15% of acute myeloid leukaemia patients survive ten or more years
Cambridge has a history of making huge strides in cancer research, from pioneering work that led to our ability to rapidly sequence the DNA of tumours to the manufacture and use of monoclonal antibodies, a technology that now underpins routine cancer therapy globally, and the development of a new generation of cancer drugs known as PARP inhibitors.
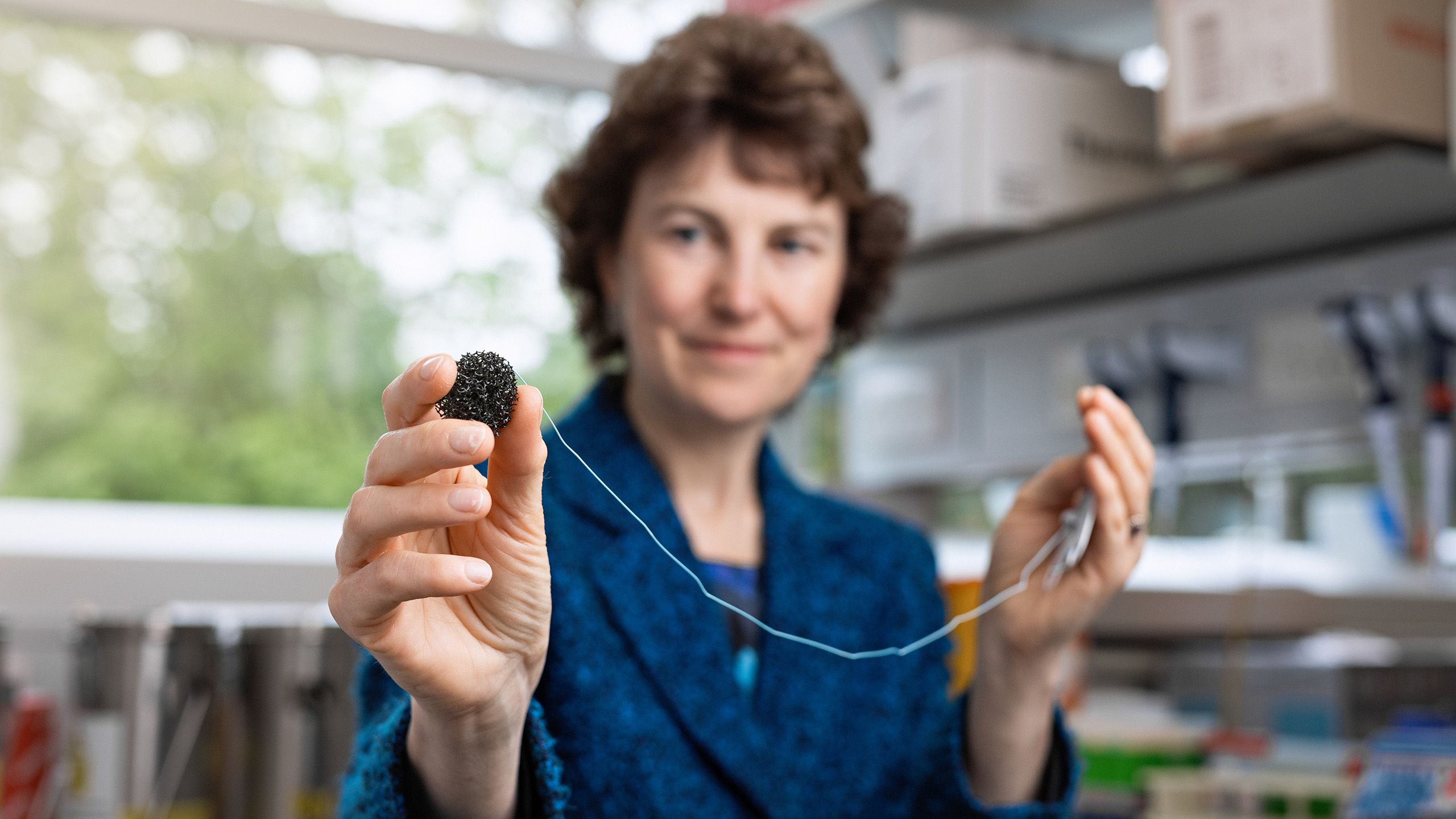
Fitzgerald’s own area of expertise is oesophageal cancer, where she pioneered the Cytosponge – a ‘pill on a string’ coupled with a lab test that is a remarkably straightforward but effective way of helping determine whether heartburn patients have Barret’s oesophagus, a pre-cursor to cancer, or are developing malignancies.
Now, she wants to build on Cambridge’s history of discovery and innovation and apply it to early cancer.
The Institute houses scientists from a broad spectrum of disciplines across the University – from biologists and clinicians to engineers, physicists and social sciences – working together under one roof to understand the fundamental biology of how cancer develops and how it evolves, and applying that knowledge to pioneer new methods for detecting, treating – even preventing – cancer early.
The Institute is located on the Cambridge Biomedical Campus, where its close proximity to a number of world-leading academic, NHS and industrial partners will prove essential to its success. These include the Cancer Research UK Cambridge Institute, the Stem Cell Institute and the Victor Phillip Dahdaleh Heart and Lung Research Institute, three hospitals, and major pharmaceutical companies AstraZeneca and GSK. At nearby West Cambridge, physicists, engineers and mathematicians will also collaborate with the Institute’s teams, and a short drive away is the Wellcome Sanger Institute.
Also on the horizon is a major new hospital on the Campus – Cambridge Cancer Research Hospital, which aims to begin construction later this year. Discoveries and innovations emerging from the Early Cancer Institute will underpin much of the research and treatment that takes place there and beyond, and will be complemented by a dedicated space in the hospital.
This is, says Fitzgerald, one of only four life sciences ecosystems in the world – and the largest in Europe – that provide the capability, critical mass, and integration of science and medicine to transform patient care.
Earlier this year, the Institute announced that it had received an anonymous £11million donation to support the redevelopment of the Hutchison building, where it is housed.
As a result of the donation, the building will be renamed the Li Ka Shing Early Cancer Institute in honour of Hong Kong-based philanthropist Sir Ka-shing Li and the enduring partnership between the Li Ka Shing Foundation and the University of Cambridge.
This donation will help Fitzgerald and colleagues achieve their ambitious goal.
“We’re working to move the world beyond the fear of cancer.”
Professor Rebecca Fitzgerald
Margaret's story
Heartburn – where acid from the stomach makes its way back up our oesophagus, causing a burning sensation – is a common condition and, in most cases, it is mild. But for Margaret*, a retired anaesthetist, it threatened to become something much more serious.
In 2012, Margaret was referred for an endoscopy to investigate the cause of her heartburn. She was diagnosed with Barrett’s oesophagus, where long term exposure to stomach acid damages the food pipe. For the majority of people – around nine in 10 – the condition does not progress further, but for a small number of people, it can develop into oesophageal cancer.
Margaret’s specialist took a biopsy of the tissue and was able to confirm that everything was okay, but because of the risk associated with Barrett’s oesophagus, she was to receive a three-yearly check-up.
Then COVID-19 struck.
As the NHS diverted resources to manage the pandemic, waiting times for check-ups increased. 2021 came and went and Margaret wasn’t contacted for her three-yearly check-up.
“I got a call in February [2022] to say that I would have to wait longer for an endoscopy, but that they could offer me this new sponge test.”
Margaret
The test used the Cytosponge, developed by Professor Rebecca Fitzgerald at the University of Cambridge. Margaret had been referred to Dr Sunny Kadri, a consultant at University Hospitals of Leicester NHS Trust and former research fellow in Professor Fitzgerald's lab conducting the initial trials of the device in 2010. It involves the patient swallowing a pill on a string. The pill dissolves to reveal a sponge, which is drawn back up the oesophagus. As it does so, it collects some of cells from the lining. It’s a procedure that takes a matter of minutes.
“It was a bit awkward to swallow, but with plenty of water goes down okay,” explains Margaret. “But it’s not as unpleasant as an endoscopy and is faster and easier, which is better for you as a patient and better for the hospital.”
The cells are stained using a laboratory marker called TFF3, allowing them to be examined under a microscope. This time, the test showed early evidence of dysplasia, a pre-cancerous stage.
Oesophageal cancer has poor outcomes – only one in eight oesophageal cancer patients (12%) survive for ten or more years, so catching the disease early is crucial. Fortunately for Margaret, the Cytosponge test had detected her condition in time for it to be treated. Dr Kadri carried out an endoscopic resection, a procedure to remove the pre-cancerous tissue. She now has three-monthly check-ups and has been told that if the dysplasia doesn’t return, it may be possible to ‘burn off’ the Barrett’s oesophagus tissue.
All this has meant that, aside from some discomfort associated with the resection treatment, Margaret is able to return to enjoying her retirement and passions of playing golf and tennis.
*Name changed at the request of the patient
DNA detectives and fossil hunters: The Early Cancer Institute's researchers

Professor Serena Nik-Zainal
Professor Serena Nik-Zainal
Professor Serena Nik-Zainal
Professor Serena Nik-Zainal is a DNA detective. She uses whole genome sequencing to investigate tumour DNA, looking for mutational signatures – or ‘fingerprints’ – that can reveal what caused the mutations in a cell’s DNA that gave rise to the cancer: was it inherited, spontaneous, or triggered by something in the environment, such as sunlight or chemicals?
“Mutational signatures are the fingerprints left behind on our DNA, and just like fingerprints, each one is unique. They allow us to treat tumours as a crime scene and, like forensic scientists, allow us to identify the culprit – and their accomplices – responsible for the tumour.”
Professor Serena Nik-Zainal
Nik-Zainal has built up expertise in whole genome sequencing and analysis over the last decade or so. Now, she wants to apply this to early cancer – even to pre-cancer, for example some of the tumours that precede breast cancer, known as ductal carcinoma in situ, DCIS.
Not everybody with DCIS goes on to develop cancer, so Nik-Zainal’s team is trying to understand what sets apart those women who go on to develop cancer from those who don’t. She will be looking at whether we see the same mutational signatures in early cancers as we do in developed cancers, as this will give clues as to which signatures are important to tumour development.
At present, if a woman arrives at the clinic with a lump in her breast, she will receive a biopsy. If it turns out to be cancer, the tumour will be removed and its DNA sequenced. This is important for guiding treatment: for example, faults in inherited BRCA genes are known to put women at high risk of developing breast cancer, but tumours can develop spontaneous (or ‘somatic’) BRCA defects – whole genome sequencing of the tumour DNA will pick up these mutations and could then guide early treatment for these women.
Nik-Zainal would like to see this sequencing happen at an earlier stage: “Maybe what we should be doing is sequencing at the start, when the patient first comes to biopsy – taking that sample, sequencing it, then really understanding at that point what is the status of the genome and is there anything we can do about it sooner? We're trying to push the boundaries, make the genome sequencing matter sooner and faster.”
Dr Jamie Blundell
You might not expect to find fossil records in a cancer institute, but this is how Dr Jamie Blundell – an evolutionary biologist by training – describes the samples he works with.
His research involves looking at blood samples taken from patients with blood cancers such as acute myeloid leukaemia (AML) many years before their diagnosis.
“If I know that someone has got cancer today, but I have this kind of ‘fossil record’ of their blood samples taken over the last 20 years or so, then I can go back to the ones taken five, 10, 15 years ago and see if I can spot the earliest signs of cancer, the signs that this person was on the road to cancer.”
Dr Jamie Blundell
Blundell uses insights from evolution and applies them to cancer, looking at how somatic mutations are acquired and expand.
“What we know about most cancers is that they're driven by the accumulation of multiple genetic changes on top of each other. What the samples enable you to do is essentially watch that process of evolution occurring, seeing how it unfolded in that person over the decades.”
To do this, Blundell takes the cancerous tissue and looks for the tell-tale genetic changes that gave rise to that cancer. He then tracks back through the older samples to see how and when the mutations arose, how they expanded and how they acquired further mutations.
Blood cancer is particularly suited to this approach, he says. “People don't come in and give you a chunk of liver or lung, but they will give you a blood sample. It's the one tissue where you can actually watch very precisely how cancer was born. And a lot of the work has pointed to the first mutations occurring very early on in your life, often in your teens.”
Blundell believes we are not far off being able to take blood samples from at-risk groups – over 50s, say – and look for genetic anomalies that suggest an individual is at a significantly higher risk of developing an aggressive blood cancer. These individuals could then be screened at regular intervals.
But detecting cancer early is only useful if something can be done it. Fortunately, there are experimental trials taking place in the US that might result in new treatments.
“This is where the detection and the treatment go hand in hand, because the very thing that you're using to detect it, which is the genetic change, will also inform your treatment. If you have a particular mutation in this gene, say IDH1 or IDH2, then there may be a targeted therapy for mutations in that gene, and so you can selectively target the premalignant condition.”

Dr Jamie Blundell
Dr Jamie Blundell

Dr Matt Hoare
Dr Matt Hoare
Dr Matt Hoare
While in the UK rates of most cancers are stable or declining, there is one cancer that is on the increase: primary liver cancer.
“Most people haven’t heard of primary liver cancer because historically, it's not been terribly common in this country. It's actually the fourth biggest cause of cancer related death worldwide.”
Dr Matt Hoare
The reason we may not have heard about it is because liver cancer only tends to occur in individuals with liver disease, where the major risk factors have traditionally been excessive drinking and hepatitis B or C, and the latter diseases are uncommon in the UK. But there is another significant risk factor: type 2 diabetes – and cases of this disease have increased dramatically in recent years, driven by rising levels of obesity.
By the time Hoare sees liver cancer patients, he says it is often too late to treat them. “We should have caught them much, much earlier, identified that they were getting liver disease and then liver cancer.”
People in the UK with chronic liver disease are currently offered an ultrasound scan every six months, but Hoare describes this surveillance programme as “fantastically expensive, but generally ineffective”.
Like Nik-Zainal, Hoare wants to harness the revolution in genome sequencing to help understand liver cancer and who is going to develop it.
Tumours are essentially clones: a cell acquires a mutation, divides and replicates, spreading while continuing to acquire new mutations. If you sequence any part of the cancer, you should find the common mutations that led to its transformation; sequencing of non-cancerous tissue is much harder.
Working with Dr Peter Campbell from the Wellcome Sanger Institute, Hoare sequenced tissue from patients with chronic liver disease and compared this to tissue from patients with primary liver cancer, expecting to find the same mutations. But this was not the case.
“What we did find [in the case of liver disease] was lots of other mutations, and we kept seeing them again and again in the same genes and in the same parts of the same genes, which tells you that there must be Darwinian natural selection taking place.”
Just as the wing evolved independently several times – in mammals, birds and insects, for example – because it carried an evolutionary advantage, then this must also be the case with these mutations, he says: they must be overwhelmingly advantageous in liver disease.
“Why is that? What does it mean for the cancer development? At the moment we just don't know. We know they’re not cancer-causing mutations, but we keep finding them in patients who are at risk of cancer. What they actually do is they seem to affect metabolism genes, they affect things that control fat, that control diabetes, that control sugars, those kind of things. They’re not immediately obviously connected to cancer, so what's the link? That’s what we aim to find out.”
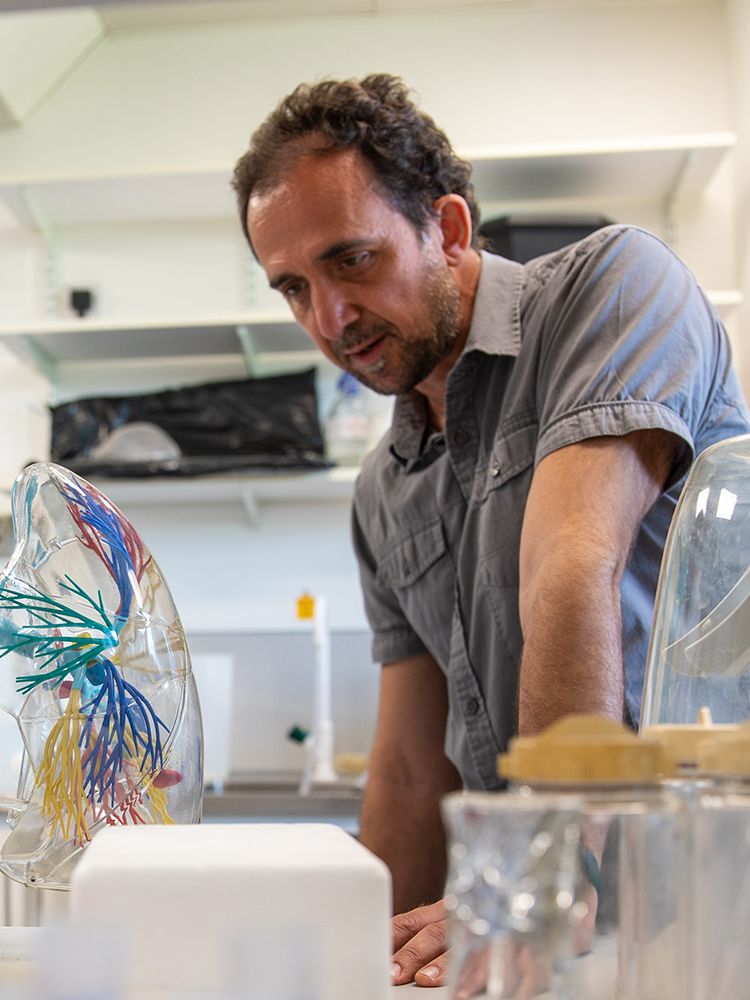
Dr Daniel Munoz-Espin
While mutations in our DNA may drive cancer, as Dr Daniel Munoz-Espin points out, “they are not sufficient to initiate cancer”.
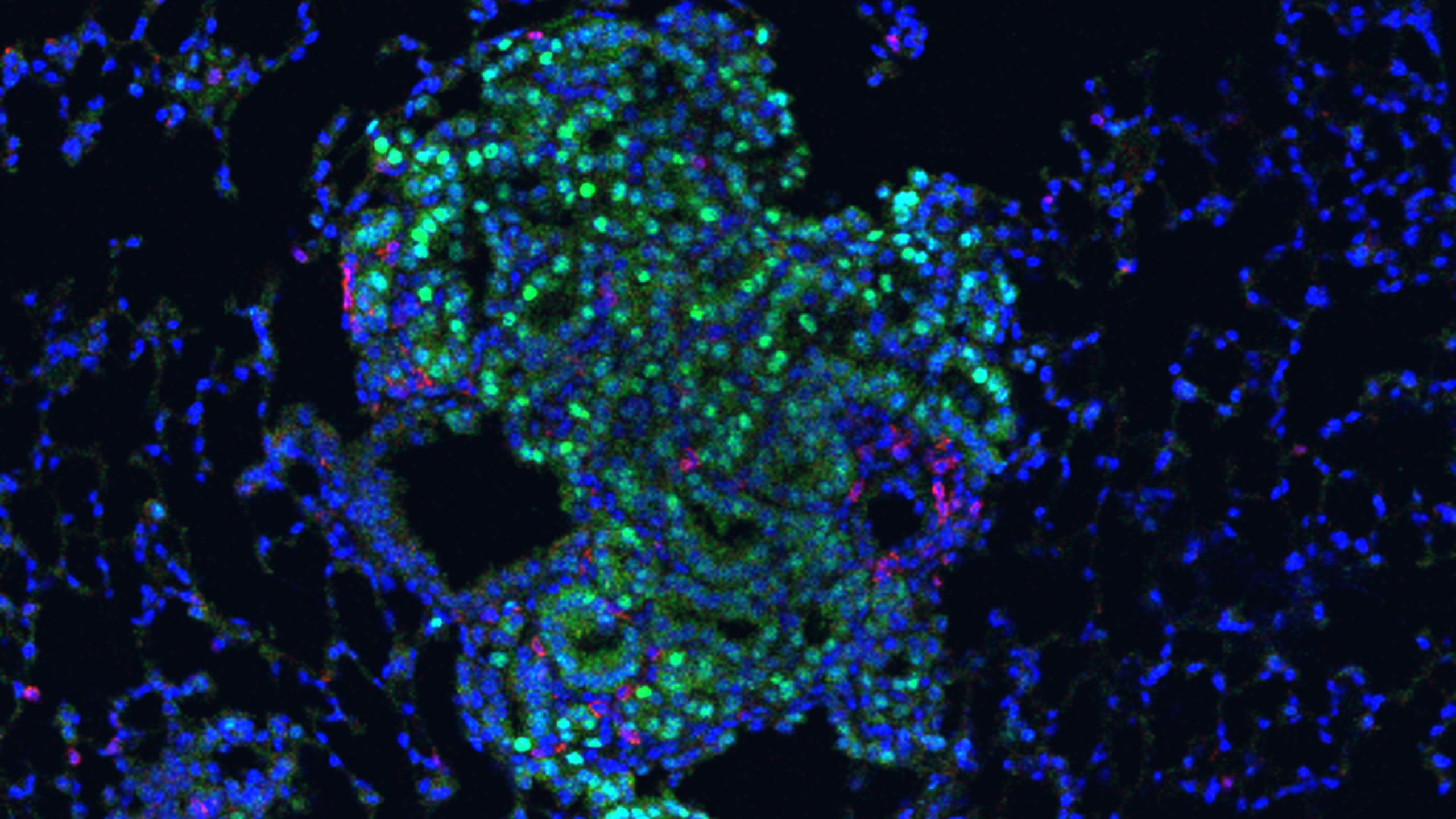
He is interested in emerging evidence that a tumour’s ‘microenvironment’ plays a fundamental role in cancer. The microenvironment is a tumour’s immediate surroundings: the blood vessels, immune cells, fibroblasts, for example. Understanding the changes in the microenvironment that enable the cancer to progress will be important for helping develop new ways to treat cancers.
“If we can target not only these cancer cells, but also the tumour microenvironment, we will be in a good position to develop more efficient and specific treatments.”
Dr Daniel Munoz-Espin
Munoz-Espin focuses on lung cancer, and among the tools he uses are organoids – ‘mini-tumours’ grown from cancer cells that mimic the behaviour of the tumour and its microenvironment. They are increasingly used to replace the use of animals, such as mice. They can also be used to screen potential drug candidates at a scale that would neither be practical nor ethical using mice.
One particular area that Munoz-Espin is interested in is senescence, one of the ways our body responds to unrepairable damage and stress, whether that be DNA damage, activation of cancer genes or response to chemotherapy drugs, for example. “Senescence is a hot topic in cancer at the moment.”
Ordinarily, cells divide and replicate, which could be problematic if the cells are damaged. Senescence prevents the cell from dividing anymore. But it does not kill the cell, and there is increasing evidence that senescent cells can have very potent tumour-promoting activity, causing cancer initiation, progression and relapse or metastasis. This is why senescent cells are often known as ‘zombie cells’, as they are supposed to be dead, but remain very much alive.
Experimental clinical trials are underway to validate ‘senotherapies’ – a cocktail of pharmacologically-active drugs that specifically target and kill senescent cells.
“We call it a ‘one-two punch’ therapy,” says Munoz-Espin. His team is trying to identify the ideal combination for lung cancer. “We’ve found that if we eliminate senescent cells, either in the precancerous stages or after chemotherapy, then we can prevent cancer initiation and progression, significantly increasing survival rates.”
Dr Daniel Munoz-Espin
Daniel Munoz-Espin (right)

Support cancer research at Cambridge
Cambridge hosts a cancer research community responsible for globally significant breakthroughs and innovations.
Together we are changing the way cancer is treated. Our scientists will make discoveries alongside expert clinicians treating patients, drawing on the world-leading expertise found within the University and across the Cambridge Biomedical Campus.
We will find cancer earlier and treat it better. Join us.

This article was first published on 21 September 2022. It was updated to include details of the £11m donation on 24 July 2024 and republished as part of the University of Cambridge's campaign Cambridge is Changing the Story of Cancer.
Photography:
- Main image of Rebecca Fitzgerald by Mike Thornton (Stillvision)
- All other images by Lloyd Mann
The text in this work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License
