Supertroopers
A life-saving cancer therapy is being scaled up in Cambridge to deliver more treatments to more patients for more cancers.
It works by super-charging the patient’s own immune system.
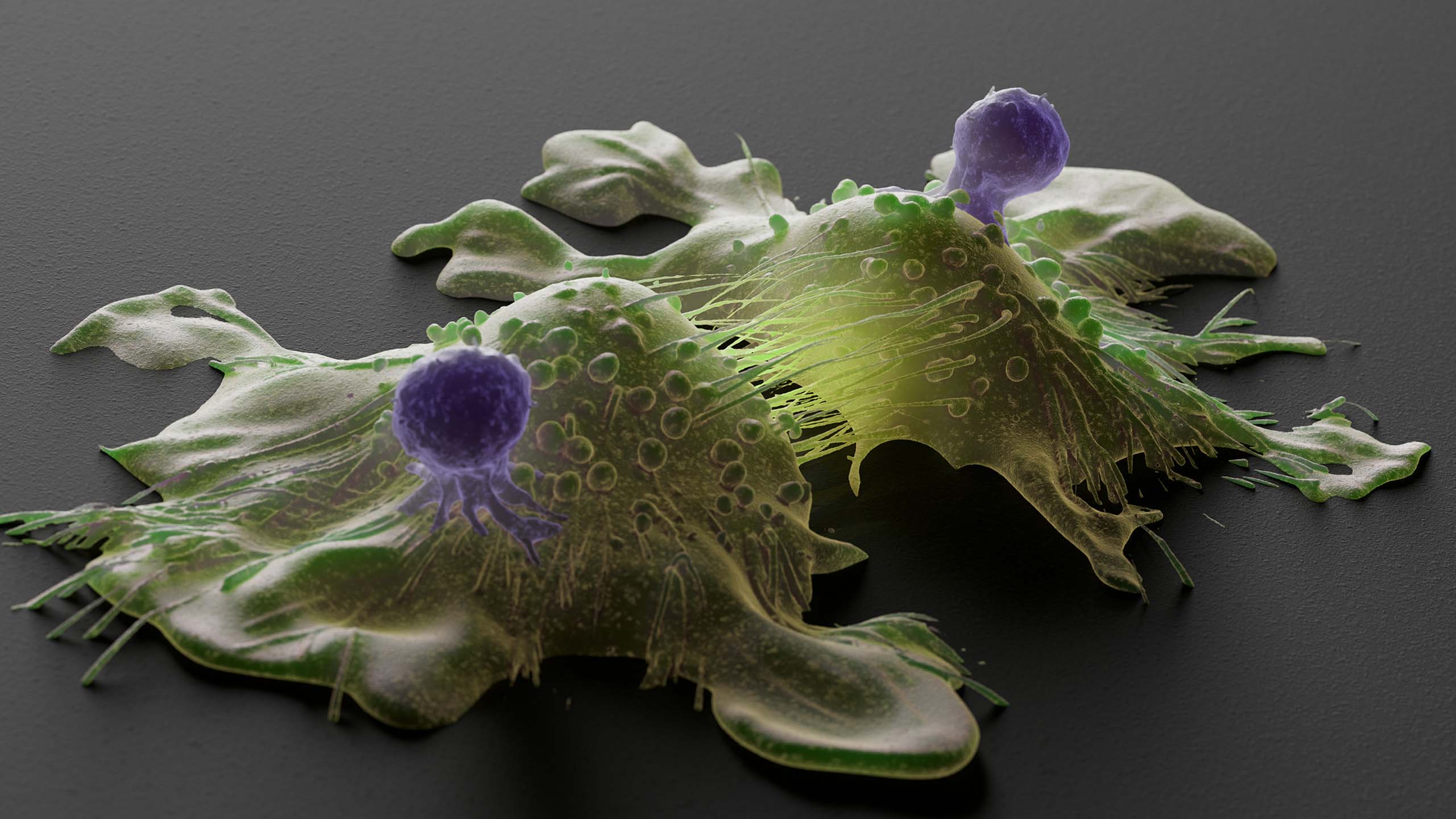
Our immune system has billions of ‘T cells’ which recognise and destroy cells that might pose a threat to our wellbeing, such as those that show specific hallmarks of infection and disease. But these remarkable cells appear to be outwitted by cancer cells, which evade detection and grow uncontrollably.
CAR-T is a type of immunotherapy that provides a way round this by turning a patient’s own T cells into a battalion of highly targeted killers.
In 2020, Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Foundation Trust, became one of only a small number of centres in England equipped to provide this complex treatment.
For some of these patients, the treatment has cured them of their cancer.
“CAR-T cell therapy is a ‘living treatment’ in that once the cells are given to a patient, they persist for many months or even years, ready to attack the cancer cells should they pop up again,” explains Dr Ben Uttenthal, clinical lead for immune effector cell therapies at Addenbrooke’s and the Cancer Research UK (CRUK) Cambridge Centre’s Cancer Immunology Programme.
“For some types of aggressive cancer we are finding that we can cure more than double the number of patients using CAR-T cell therapy. It’s been a game-changing treatment – and we’re only just scratching the surface of what’s possible.
“All the parts of the jigsaw are now coming together to develop newer and better therapies in Cambridge so that we can get more people back into the life they want to live.”
What is CAR-T cell therapy?
Blood is collected from the patient and their T cells are isolated.
The T cells are then reprogrammed to carry a protein called the chimeric antigen receptor (CAR), which recognises certain cancer cells.
These modified CAR-T cells are then grown into large numbers and given back to the patient.
When the CAR-T cell spots a cancer cell, it starts to multiply and attract other parts of the immune system to attack and kill the cancer.
A 'living treatment' for patients
After receiving CAR-T cell therapy at Addenbrooke’s Hospital, one patient credited the treatment with saving his life.
“I was basically told there was nothing else that could be done [for my leukaemia] as far as conventional medicines were concerned. It was at this point my consultant told me about a new trial that was taking place known as CAR-T cell therapy. For me it was the last chance saloon,” said Steve Johnson.
“Having the treatment is not pleasant – I had a number of fevers and temperature spikes for two weeks after the CAR-T cells were put back in, but I have absolutely no doubt this treatment saved my life.”
So far, only some types of blood cancers have been approved for CAR-T cell therapy by the NHS, explains Uttenthal: “The pioneering treatment is currently being offered to patients with aggressive forms of blood cancer called B-cell lymphoma and acute lymphoblastic leukaemia who have either relapsed or not responded well to chemotherapy or stem cell treatment.”
One such patient was a 54-year-old woman with a B-cell lymphoma which had shown no response to several different types of chemotherapy.
“After we infused the CAR-T cells back into her, the cells became activated and attacked her lymphoma,” says Uttenthal.
“The reaction was so vigorous that at one point we needed to give an antidote to damp down the immune response. She needed intensive monitoring for a time, but after a couple of weeks she improved and she’s now completely recovered. The last time we spoke she was away on a golfing trip in the Mediterranean!”
Dr Ben Uttenthal (credit: Dr Claire King)
Dr Ben Uttenthal (credit: Dr Claire King)
The number of patients who can benefit from CAR-T cell therapy is increasing, explains Uttenthal: “That’s partly because the success of CAR-T cells has meant that they are being brought to earlier lines of treatment.
“But we want to increase this yet further by implementing CAR-T cell therapy for other kinds of cancer, and by making CAR-T cells that have fewer side effects so that they can be given in less specialist centres.”
To improve CAR-T cell therapy further needs experts like Dr Mike Chapman, whose work at the MRC Toxicology Unit in Cambridge has focussed on identifying new targets and reducing toxicity.
New targets, less toxicity
Dr Mike Chapman is an expert in proteomics – the study of the interactions and structures of proteins and their cellular activities – and is the “academic driver behind what we do” says Uttenthal.
One focus of Chapman’s work has been myeloma, a cancer of a type of white blood cell called plasma cells. “Although CAR-T cells have been developed for this cancer, they haven’t yet given the long-term responses that we have seen in other blood cancers,” he explains.
Dr Mike Chapman (credit: Dr Claire King)
Dr Mike Chapman (credit: Dr Claire King)
Taking samples of tumour from patients with myeloma, Chapman has been using proteomic techniques to map and quantify the many thousands of proteins on the surface of these cells – and then using computational approaches to prioritise and select them as potential targets.
Having multiple targets will be better than just one, adds Chapman, “otherwise, the cancer will always find ways to escape.”
He is currently working with CRUK’s innovation arm, Cancer Research Horizons, to progress the most advanced of the targets he’s identified into effective treatments for cancer patients.
“There’s a predictability about CAR-T cell therapy,” adds Chapman.
“With blood cancers, if you know the target on the cancer cell and you can make the CAR-T cell that will target it, then these living therapies are essentially curative. And we also know that if some off-target killing of normal blood cells happens then the patient’s blood system copes well.”
But, in the case of myelomas, current therapies have run into problems whereby the CAR-T cell accidentally targets cells in the brain tissue. Chapman is working on a potential solution: ‘on-off gates’.
“We can make CAR-T constructs clever enough to switch themselves off if they recognise a marker that identifies it as the wrong cell to kill – like a brain cell,” he explains.
“But we’re taking this a stage further by re-wiring the cell to attack cancer cells that express only low levels of the target. It’s a complicated system but the great thing about CAR-T cells is it’s a ‘rational therapy’ – what you predict happens actually does happen.”
Making CAR-T ‘in house’
CAR-T therapy is expensive because both the engineering of the cells and the manufacturing is carried out by specialist companies. Sarah Albon is looking to bring this home.
Albon is the director of the Cambridge Cellular Therapy Laboratory (CCTL) at Addenbrooke’s Hospital. She leads a team with expertise in immunotherapies and delivering bone marrow and stem cell transplants across the whole of the East of England.
“That’s CCTL’s ‘bread-and-butter’ job,” she says. “But we also act as a regulated cell handler for a number of other novel cell therapy products – particularly those that have just come onto the market like CAR-T cells.”
Currently, the CAR-T cell therapies are manufactured by large pharmaceutical companies. Albon’s team delivers the patient cells to the manufacturer and then receives and stores the final T cell product ready for when the patient needs it.
“These novel products are made specifically for each patient from their own cells, so we have to be 100% sure they are what we think they are to make sure that each patient receives the correct treatment. This is why the work we do in CCTL is highly regulated.”
A state-of-the-art clean room suite is being built on the Addenbrooke’s site that will expand the facilities of CCTL significantly. The aim is to deliver more treatments to more patients for more cancers, in readiness for the planned Cambridge Cancer Research Hospital being built.
The expansion will also mean a greater capacity to be involved in clinical trials.
“A CAR-T might be licenced for use in acute lymphoblastic leukaemia for example, but in order for that same product to be used in a different malignancy, it would have to undergo a clinical trial in that patient population. Then the manufacturer gathers the data and applies for a licence,” she explains.
Sarah Albon (credit: Nick Saffell)
Sarah Albon (credit: Nick Saffell)
“We already work closely with the Cambridge Clinical Trials Centre at Addenbrooke’s on CAR-T trials and we will be expanding this once the new labs are up and running.
“Our ultimate goal is to manufacture our own CAR-Ts in our own laboratories here in Cambridge. The expertise and infrastructure are in place, and our new expanded facilities will enable us to do that. It's now within reach.”
Support cancer research at Cambridge
Cambridge hosts a cancer research community responsible for globally significant breakthroughs and innovations.
Together we are changing the way cancer is treated. Our scientists will make discoveries alongside expert clinicians treating patients, drawing on the world-leading expertise found within the University and across the Cambridge Biomedical Campus.
We will find cancer earlier and treat it better. Join us.

Published: 16 October 2024
Words: Louise Walsh
Images: banner image credit Thom Leach/Science Photo Library via Getty Images; CAR-T diagram credit ttsz via Getty Images; others as shown
The text in this work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License





