COVID-19: What to expect from a vaccine
By Gordon Dougan

One of the hottest topics around COVID-19 is the need for a vaccine for this new disease, which has had a huge impact on both human health and economies. The disease caught most people completely by surprise and shows no signs of disappearing naturally. In many ways the consideration of health and economics form the two extremes of a risk assessment of how to manage the outbreak and minimise the impact.
Vaccines have tremendous attraction in that they can protect those who have not already succumbed to the infection. They could, in theory, end the pandemic and give people long-term reassurance that the health risk has been diminished or removed. Vaccines are the silver bullet.
However, vaccines are also not welcomed by everyone. Administering a preventative medicine means you are exposing potentially healthy people to risk even if it is incredibly small. Also, even if a vaccine works, the benefits are not immediately obvious to those vaccinated or those close to them such as parents. For these reasons, much of the development of new vaccines in recent decades has focused on safety and more safety. This comes at a huge cost, is incredibly time consuming, but is essential.
Safety issues often only emerge towards the end of the vaccine development cycle as they can be relatively rare events. So vaccines often fail only after vast amounts of money have been spent. This means that vaccine production now rests with the few organisations able to bear these costs and risks, usually large pharmaceutical companies.
THE CANDIDATES

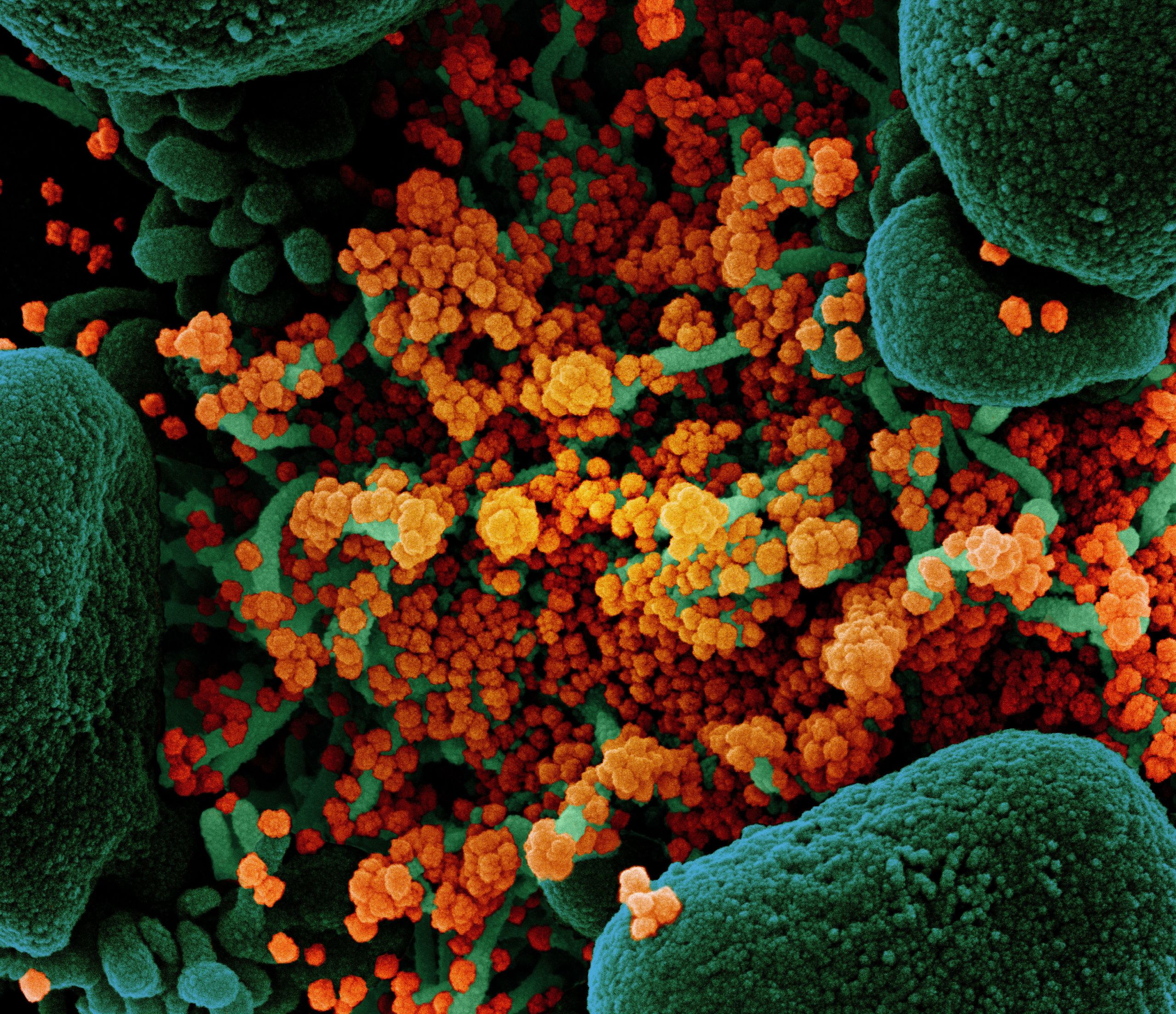
COVID-19 is caused by the novel coronavirus SARS2-CoV-2. This is in itself an issue as we currently have no licenced human vaccines that work against coronaviruses. We have to start more or less from scratch.
Over the past decade we have been dealing with other coronaviruses that have caused restricted outbreaks, such as the MERS and SARS1 viruses. However, these were controlled using classical outbreak management and no licensed vaccine was developed against these viruses.
However, licensed vaccines were developed against Ebola. Although this is a different type of outbreak virus, it stimulated the formation of organisations such as the Coalition for Epidemic Preparedness Innovations that started to plan to make vaccines against known and potentially unknown outbreak viruses.
There are now over 100 COVID-19 vaccines in different stages of development and they come in many forms. I have written a blog that reviews not only the vaccine types but also outlines the potential steps that have to be navigated in order to get a vaccine licensed.
It is no accident that one of the most advanced COVID-19 vaccines benefits from work already in place on Ebola. The team at Oxford University who have been developing and testing their vaccine were well set to simply switch their system from Ebola to COVID-19, and they did this effectively.
Teams in China are also developing vaccines based on growing and inactivating the actual SARS2-CoV-2 virus, and US company Moderna, along with scientists at Imperial College London are taking a more novel approach using ‘genetic vaccination’ based on gene delivery to fool the body into producing virus components and raising immunity.
Cambridge, too, has now entered the ‘race’ to develop a vaccine, using a different approach – synthetic DNA to deliver custom designed, immune selected vaccine antigens. If successful, it could begin clinical trials in the UK early next year.
BBC Look East's Richard Westcott meets the team at the University of Cambridge who are developing a vaccine against COVID-19
These different types of vaccines present different opportunities, risks and challenges.
RISK ASSESSMENT

The fact that SARS2-CoV-2 is such a new virus means we have not developed any indirect measurements of ‘protection’. For some other vaccine classes we have developed ‘immunological correlates of protection’ - in other words, measurable signals in the body that indicate protection has been achieved.
Therefore, the only real way of actually proving a COVID-19 vaccine works is by measuring directly if it protects humans against (a) SARS2-CoV-2 infection itself and/or (b) clinical disease (in other words, COVID-19). Obviously, prevention of infection is the gold standard but is often not easy to achieve.
Also, vaccines often only give partial protection, protecting some but not others (we call this the efficacy of the vaccine). An ideal vaccine would give close to 100% protection, but often it is lower than this - even 50% protection is sometimes acceptable. This is because even a vaccine of relatively low efficacy can sometimes induce ‘herd immunity’ by limiting the transmission of the virus in the community.
We will need to risk assess each vaccine as it is developed. Normally, regulatory authorities are the key organisations that decide if a vaccine can be licensed for use in a country. In the UK this is the Medicines and Healthcare Products Regulatory Authority (MHRA). Such regulators will usually insist on all possible safety and efficacy measurements are assessed. However, regulators, working with governments can waiver these requirements and license a vaccine with more limited data. This is happening in Russia with the Sputnik V vaccine, prompting some concern that a largely unproven vaccine is being rolled out to a large number of people.
A compensating approach would be to continue to collect safety and efficacy data after licensing. This is the dilemma we all face with the COVID-19 vaccine race. It is compounded by the fact that many of the vaccine approaches proposed for COVID-19 have not been extensively validated for safety over long periods in a variety of social groups (for example children or the elderly) or settings (such as different populations).
GETTING THE VACCINE TO THOSE WHO NEED IT (AND WANT IT)

Despite many claims, it will take some time to resolve safety issues and to manufacture large amounts of a vaccine and distribute it effectively to those who need it. When we do have a vaccine, where should we start? Many of these issues will be handled on a vaccine-by-vaccine and a country-by-country basis. Nevertheless here are some considerations.
Who to vaccinate first. It is normal practice to start any vaccine campaign with healthy adults. They would be expected to respond to and tolerate a vaccine better than other groups. I would anticipate the initial vaccination of healthcare workers, teachers or other people likely to be most at risk to virus exposure.
Babies and toddlers. Even though young or even newly born children are frequently the target of vaccination they are always one of the last group to be vaccinated during ‘normal’ vaccine development. There immune system is still developing and babies may have received protective antibodies from their mother. I anticipate a delay in vaccinating very young children, particularly as they appear to be less susceptible to disease.
The elderly. Clearly the older you are, the more at risk you are to COVID-19. However, elderly people frequently respond less well to vaccination and special vaccine formulations may be required e.g. they may need an ‘adjuvant’, which activates the immune system and can stimulate protection in individuals who would normally not respond or be protected. Specific studies will be carried out in the elderly.
Other vulnerable populations. Certain groups or cohorts such as diabetics or obese individuals appear to be more vulnerable to COVID-19. These individuals may be targeted early for vaccination but they will need specific clinical consideration and perhaps special vaccine formulations.
Ethnic minorities. There is evidence that some ethnic minority groups may be more susceptible to COVID-19 although the factors driving this remain largely undefined. These groups may be targeted as a priority.
Lower income countries. Few countries have the ability to make vaccines and even fewer can afford to pay for expensive products. Thus, we will need to design vaccines that are effective, safe but also affordable. This is a special art in itself unless companies are willing to sell vaccines at low prices.
WHAT NEXT?
We are now right in the middle of watching the development of new vaccines in real time. It will be very interesting to see how all of this unfolds over the next months and years. We can anticipate some scares and some vaccines dropping out of the race. We will see a scramble to vaccinate once supplies start to come on line, with richer countries potentially buying up much-needed supplies and leaving poorer countries empty-handed. Key political decisions will have to be made.
It will still take several years to see if vaccination really works and is absolutely safe. Whatever the outcome, we need to learn from this pandemic and be ready for the next one as it will be coming.
Gordon Dougan is a Professor at the Cambridge Institute for Therapeutic Immunology and Infectious Disease, University of Cambridge, and has spent his career leading research into vaccines, pathogen genomics and disease tracking. His research work has helped to redefine our understanding of how infections spread around the world, a subject of direct relevance to the current COVID-19 epidemic. He was recently awarded the Albert B Sabin Gold Medal Award for work in vaccinology.
Image credits
SARS-CoV-2 model and vaccine syringe (pearson0612)
Syringe and vials (qimono)
Vaccination (kfulhert)
Child being vaccinated (Public Health Image Library, Centers for Disease Control and Prevention)
Novel Coronavirus SARS-CoV-2 (National Institutes of Health)

