“Behind every COVID-19 test sample is a person worried about their results”
Meet the volunteer scientists who turn swab samples into diagnoses – again and again and again.

It’s 5:45am and a small band of scientists are leaving their flats to cycle through the silent streets of Cambridge ready to start the 6:15am shift at the Cambridge Testing Centre, set up in partnership with AstraZeneca and GSK.
Once through the doors of the Cambridge Testing Centre they will put on full PPE and stand in an air shower for 10 seconds, before stepping over the threshold into the lab.
And now our volunteers are ready to begin testing swab samples for COVID-19.

We know that testing for COVID-19 is important. But what many of us may not know is how the process actually works. We meet the volunteers behind the testing, who explain how you go from swab sample to diagnosis.
Stage one: sample preparation
“The process of analysing samples is split into several steps,” explains Dr Martin King, a laboratory manager at the MRC Mitochondrial Biology Unit. “I work in a team that carries out the first stage of this analysis.
“The samples are delivered to the COVID-19 Cambridge Testing Centre and our first job is to assess every vial to make sure that it's safe and suitable for analysis.”
The team pipette each sample into what is known as a 96 well-plate before adding a chemical that neutralises the virus. Finally, the samples are put into a 65-degree oven for 10 minutes – this deactivates the virus so that it is no longer harmful but can still be detected from the PCR test.

Sample preparation team at work
Sample preparation team at work
The tasks are routine and yet require unwavering concentration. The volunteers work quickly and carefully to process as many samples as possible.
“I lose count of the number I've processed pretty quickly,” laughs Undine-Sophie Deumer, “and so the best moment of the day is when we are told the number of samples we have processed during our shift, because behind every sample is a person worried about their results.”
Volunteering was a very natural step to take for Deumer, a Research Assistant at the Department of Pathology, having long been interested in the area of disease diagnostics.
“The reason I went into this field was to improve people’s lives. We have a real opportunity to increase the number of tests being carried out and successfully diagnose people. I’m glad I can help the NHS and be part of the solution to this global health emergency.
“I have friends and family for whom this virus is likely to be much more dangerous than for me, so volunteering at the Cambridge Testing Centre also means making the world a bit safer for them and everyone else at risk.”

Undine-Sophie Deumer
Undine-Sophie Deumer
For King it was witnessing first-hand the dedication of NHS staff that led him to volunteer. “My sister is a Ward Manager at Addenbrooke's Hospital. She was typically working 60-70 hours per week, while I was just sitting at home with very little to do, because my lab had closed. I felt so frustrated not to be able to help, and so when I heard that the University was looking for volunteers, I jumped at the chance to get involved.”
Stage two: RNA extraction
“RNA extraction is a highly automated process” says Dr Veronica Caraffini, a postdoctoral researcher at the MRC Cancer Unit. “The first task of the day is to prepare the reagents to be used in the RNA extraction, and then to set up the robots which will carry out the process.”
“Next we’ll receive a call from the sample preparation team who tell us how many 96 well-plates they have for us to process. These plates will go into the robots which carry out the extraction. The end result is a further plate of purified RNA samples.
“When we first began testing, each robot was able to process two plates at a time, however we’ve been working to enhance their capacity – now all of our robots can process three plates at a time.”

Dr Veronica Caraffini conducting RNA extraction
Dr Veronica Caraffini conducting RNA extraction
For Dr David Gershlick, a Sir Henry Dale Fellow at the Cambridge Institute for Medical Research, it’s these adaptions and improvements which make the work particularly rewarding. “It’s really exciting to see that we’re making huge leaps in efficiency,” says Gershlick. “Every day we are honing the process both in terms of running the machines and how we work as a team.”
For Gershlick and so many of the volunteers at the Cambridge Testing Centre, the opportunity to be part of such a tight-knit and purposeful team has been incredibly rewarding. But just as importantly, it has provided much needed company for volunteers who are living alone or are new to the city.
This has been particularly true for Caraffini who, having moved to Cambridge at the end of last year, had only a few months at the University before lockdown began.
“I love the environment at the Cambridge Testing Centre – it’s so stimulating,” says Caraffini. I like the way people with different backgrounds and diverse jobs have come together to tackle this difficult situation.
“The situation we live in is unusual, and can be scary and unsettling. But being part of something bigger, and seeing what people can do in such a short time to be of help, is inspirational.
“And, of course, I like to think that, even if only in a very small way, I’m giving my tiny contribution to this unprecedented fight.”
Stage three: RT-PCR
“The final laboratory-based stage is called RT-PCR (Real-time Polymerase Chain Reaction), says Dr Franck Dumetz, a Research Associate at the Department of Pathology. “PCR allows genetic material to be amplified which means if the virus is present, it can be detected.
“Each robot can process 384 samples (four plates) at a time” says Dumetz. We’d never be able to process so many samples manually in one day.
“This particular technique, PCR, is very common in my field. However, we hardly ever need to use machines to set the reactions up. I’ve never had to handle so many samples at once. What blows my mind is the automation of the process. I'm not sure I will ever agree in the future to fill up a 384-well plate manually!”
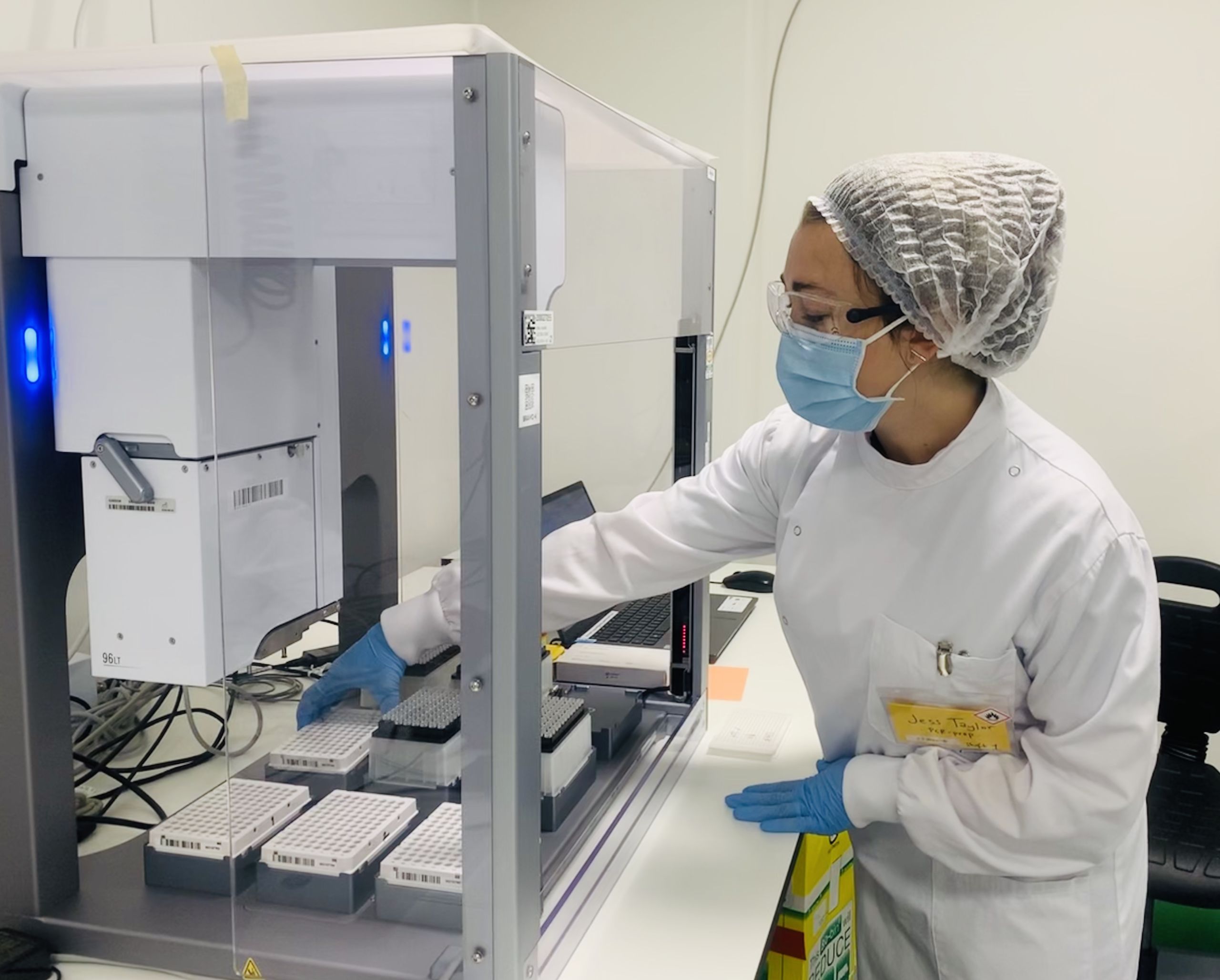
Dr Jessica Taylor conducting RT-PCR
Dr Jessica Taylor conducting RT-PCR
Having used robots previously to carry out PCR tests as part of her PhD, Dr Jessica Taylor, felt it was her duty to use her experience and skills to volunteer at the Cambridge Testing Centre.
“As soon as I heard AstraZeneca and GSK were collaborating with the University to help boost national testing, I knew I had to volunteer based on my experience and skillset,” says Taylor, a Postdoctoral Associate at Cancer Research UK. “I became a scientist to help people, I have to pause my research for now, so this is the best way to do that.”
Dumetz agrees: “While fundamental research takes years to be done properly, and even longer to see an application of it, here I have the opportunity to put the skills directly at the service of people’s health.”
And for Taylor there is another reason to volunteer close to her heart – her family. “Many members of my family are shielding due to recent cancer treatment and other health issues; it’s been really hard on their mental health and knowing that I’m contributing in some way to getting them out of that situation is really important to me.”
Stage four: data analysis
“The role of the data analysis team is to identify any samples which show a positive result for COVID-19,” says Dr Ionel Sandovici, a Research Associate at the Department of Obstetrics and Gynaecology and the Wellcome-MRC Institute of Metabolic Science. “We are sent the results of the PCR which we run through specialised software.”

Dr Ionel Sandovici carrying out data analysis
Dr Ionel Sandovici carrying out data analysis
The PCR data from every plate is analysed by two members of the team, to ensure consensus in judgement. These results are fed back into the software, which is equipped with artificial intelligence (AI), thus enabling continuous improvement of diagnosis accuracy. Finally, the anonymous test results are sent back to the NHS who will pass these onto their patients.
It’s this very tangible outcome and practical way to help that has resonated with so many volunteers, all of whom are dedicated to improving the lives of others, but who may not see the practical applications of their own research for years to come.
Dr Gahee Park, a postdoctoral researcher at the Department of Oncology, (and luckily naturally a ‘night-owl’) volunteers on the 3:15pm to 12:15am shift.
“Nobody knew this was going to happen,” reflects Park. “I think this time of volunteering, as part of the national effort to combat COVID-19, will be one of the most unforgettable periods of my life.”

Dr Gahee Park with team members on a video call.
Dr Gahee Park with team members on a video call.
It’s 12:15am and the shifts of our volunteers have finished for the day. As the scientists slip out of scrubs and shut down their laptops, the city sleeps on.