Cohesion, collaboration and clinical impact are the watchwords of a new phase of stem cell research in Cambridge.
Cohesion, collaboration and clinical impact are the watchwords of a new phase of stem cell research in Cambridge.
Cambridge is one of the few places in the world that has a critical mass in both basic stem cell science and medical translation.
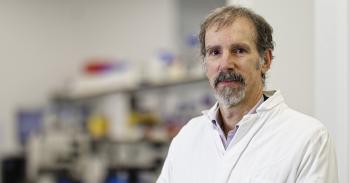
Professor Austin Smith
Few areas of research have been surrounded by such hope – and such hype – as stem cell biology. With their unique capacity to renew themselves and to give rise to the body’s many different cell types, stem cells have the potential to repair tissues damaged by disease or trauma: from a failing heart to lost nerve cells.
But the route from the laboratory to the clinic is a long one. Before patients can be treated, many years of fundamental research and clinical testing have to take place. “Rushing into the clinic without basic understanding may create some headlines but no real benefit for patients,” said Professor Austin Smith, Director of Cambridge’s Wellcome Trust (WT) Centre for Stem Cell Research. “Cambridge is one of the few places in the world that has a critical mass in both basic stem cell science and medical translation.”
Since 2007, the University has invested over £38 million in laboratories and posts, and has prioritised stem cell biology as a Strategic Research Initiative. There are now 26 stem cell laboratories across the University, which have attracted some £95 million in funding. Many of the researchers are hosted by the WT Centre and the University’s Medical Research Council (MRC) Laboratory for Regenerative Medicine (established by Professor Roger Pedersen), which focus on fundamental and translational stem cell research, respectively.
Now, a major effort is under way to draw together stem cell research across the University into a new Stem Cell Institute (SCI). The SCI currently spans several sites but the intention is to bring all these groups together ultimately in a major new research institute on the Cambridge Biomedical Campus. Unification will create the ideal stage for the translation of fundamental research into clinical benefits – research such as the long-running programme led by Professor Robin Franklin in the Department of Veterinary Medicine, whose work on multiple sclerosis is about to move into clinical trials (see below).
“Collaboration has always happened in Cambridge,” explained Professor Smith, “but pulling people together will capitalise fully on the rich opportunities. SCI will provide a unified organisation and a strategic direction for stem cell research that starts from basic science but sets clinical delivery and interaction with bioindustry firmly in its sights.” A key component will be interdisciplinary research teams that link stem cell biology with molecular disease mechanisms through to clinical applications.
Alongside Professor Smith in spearheading the reshaping will be the newly established Chair of Stem Cell Medicine, to which Professor Oliver Brüstle has been elected. Professor Brüstle is currently Director of the Institute of Reconstructive Neurobiology at the University of Bonn, Germany, and an expert in stem cells of the nervous system and their application in neurodegenerative disease.
Professor Brüstle – who notably fought for legalisation of research on human embryonic stem (ES) cells in Germany and finally became the first scientist to obtain a respective license – regards stem cell therapies as “just another way to treat disease”. He is at pains to emphasise that cell transplantation is not the only way that stem cells can bring clinical benefit: “In fact, a much closer prospect is the use of stem cells to study specific diseases in the laboratory and to develop new drugs.” Another important opportunity is the possibility of improving cancer treatment by identifying and targeting tumour stem cells.
“Of course there are challenges to overcome before stem-cell-based medicine is commonplace,” added Professor Brüstle. “For example, we need to learn more about how human ES cells differ from mouse ES cells, and how their fate is controlled.”
In fact, a major discovery about the differences between human and mouse ES cells was made in Cambridge. Professor Pedersen and Dr Ludovic Vallier and colleagues showed that human ES cells represent a developmentally more mature stage than naive mouse ES cells. This can explain why some procedures for producing specific cell types from mouse ES cells do not work well with human cells. “Human ES cells are less versatile. This research has changed the way stem cell researchers think about human ES cells,” explained Professor Smith.
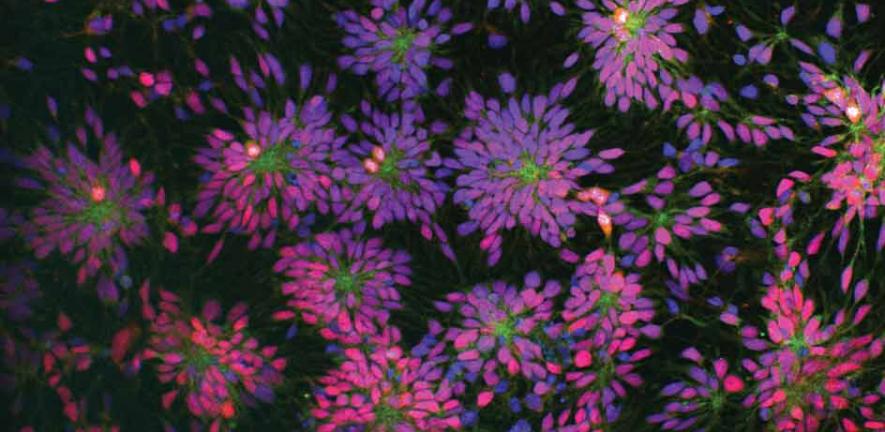
The goal now is to understand this difference at a molecular level. Professor Azim Surani at the WT/Cancer Research UK Gurdon Institute in Cambridge has pioneered a deep-sequencing technique to do precisely this. His team can now analyse the entire transcriptome (all the gene products) in a single stem cell, opening the door not only to understanding the specific nature of human ES cells but perhaps also to how to make them more like mouse cells.
Professor Smith foresees a time when stem cells will permeate all areas of biology: “Stem cells are going to be instrumental in taking us to the next level of understanding about how cells make decisions about their fate. Increasingly, we’ll see them being used in laboratories as systems to look at basic biological questions that may have nothing directly to do with stem cell biology. Stem cells will soon become the research tool of choice in mammalian cell biology.”
Self-service brain repair in multiple sclerosis (MS)
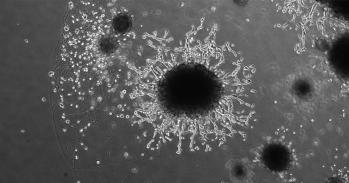
Researchers led by Professor Robin Franklin at the MS Society Cambridge Centre for Myelin Repair recently discovered a molecule that is capable of activating the brain’s own stem cells to repair damage caused by MS. Now, preparations have begun for a small-scale trial to test whether this process can regenerate lost nerve function, for which there is currently no treatment available.
Nerve fibres are progressively damaged in MS because they lose a protective coating of myelin when the cells that make it (the oligodendrocytes) are destroyed by the body’s immune system. The aim of the new treatment will be to stimulate stem cells that occur naturally in the brain and which have the ability to regenerate lost oligodendrocytes.
In the course of over two decades of research, Professor Franklin and colleagues have found that one of the major problems in MS is that the patient’s stem cells lose the ability to become normal oligodendrocytes. When oligodendrocytes are destroyed during the MS disease process, they are not replenished from the brain’s pool of stem cells. But the ability can be regained when the patient’s stem cells are activated through the retinoid acid receptor RXR-γ, as shown in collaboration with colleagues in Edinburgh using animal models and published in Nature Neuroscience in January 2011.
The discovery was a landmark moment in the search for treatments for MS, as Professor Franklin explained: “If we can encourage the patient’s own stem cells to develop into oligodendrocytes and replace the lost myelin, then this might restore the nerve functions lost in MS.”
The idea behind the proposed treatment is not only to repair the damage but also to arrest any further damage caused by the patient’s immune system. An effective treatment for halting the destruction of oligodendrocytes, alemtuzumab (Campath), was developed in Cambridge by Professor Alastair Compston and Dr Alasdair Coles at the Department of Clinical Neuroscience.
The prospective new trial, which is currently being designed by Dr Coles together with colleagues at University College London and the University of Edinburgh, and is not yet recruiting patients, plans to use a licensed drug, bexarotene, which activates RXR-γ.
Professor Franklin added: “Essentially, the philosophy of our approach is not to transplant stem cells from elsewhere but to encourage the patient’s own stem cells to do the work of repairing the damaged tissue.”
This work is licensed under a Creative Commons Licence. If you use this content on your site please link back to this page.