Researchers discover that the cells play a major role in inflammation which underlies Crohn’s disease in small intestine.
Researchers discover that the cells play a major role in inflammation which underlies Crohn’s disease in small intestine.
If we are able to break down Crohn’s disease into subsets by understanding the underlying mechanisms, which we have done here, we hope to develop much more targeted, effective treatments.
Professor Arthur Kaser
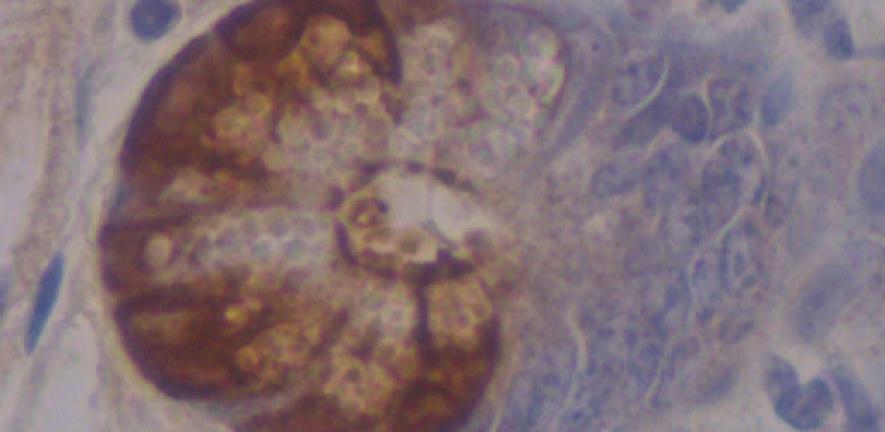
Scientists have discovered that Crohn’s disease, the inflammatory bowel disorder, can originate from specialised intestinal cell type called Paneth cells. As such, they propose that small intestinal Crohn’s disease might be a specific disorder of this cell type, providing a possible new target for treatments. The study, by researchers from the University of Cambridge and Harvard University, was published today in the journal Nature.
“If we are able to break down Crohn’s disease into subsets by understanding the underlying mechanisms, which we have done here, we hope to develop much more targeted, effective treatments,” said Professor Arthur Kaser from the University of Cambridge, one of the lead authors of the paper. “The discovery of the Paneth cells’ role in inflammation of the bowel also raises the possibility of entirely novel therapeutic approaches.”
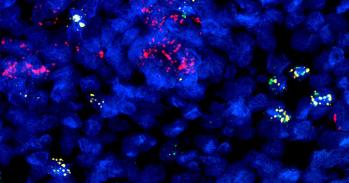
The researchers also identified the mechanism by which defects in autophagy, the breakdown and recycling of unnecessary cellular components in the body, can lead to Crohn’s disease.
Autophagy had previously been linked to Crohn’s disease - several key genes associated with Crohn’s disease play a role in autophagy - but it was not clear how. Some speculated that since Crohn’s disease develops in the intestine, where the immune system is exposed to all the myriads of bacteria in our gut, that defective autophagy might lead to Crohn’s disease via an inability to remove bacteria within the cells. However, the new research reveals that autophagy plays a role in keeping in check the inflammatory function of the unfolded protein response, which is activated when the endoplasmic reticulum (ER) is stressed.
ER stress is very common in the intestines of Crohn’s patients. The researchers speculate that autophagy may remove ER membranes which are rendered ‘inflammatory’ by the accumulation of misfolded proteins either as a consequence of genetic traits in the unfolded protein response or environmental factors (e.g. from the microbiota). The research shows how autophagy genes interact with ER stress genes, as well as with the environment, to cause disease – an important aspect for our understanding of complex diseases such as Crohn’s disease.
The researchers showed that the interaction of ER stress and autophagy could be therapeutically targeted in their model of the disease. One of the drugs they used was rapamycin, which induces autophagy. Professor Kaser commented on this approach: “A similar drug to rapamycin had been used in a clinical trial for Crohn’s disease but failed. However, we speculate that if it was studied in a specific subset of Crohn’s, that the drug might actually prove effective.”
Crohn’s disease is a debilitating, life-long immune-related disease that in the majority of patients starts in early adulthood, and involves cramping pain, diarrhoea, weight loss, urgency, perianal fistula formation, abscesses, low grade fever and has a profound impact on quality of life. Flares of the disease are followed by periods of remission, and the individual course cannot be predicted at diagnosis. It is thought to develop in genetically susceptible individuals when they are hit by - essentially unknown - environmental factors.
The prevalence of Crohn’s disease is 322/100,000, meaning that over 200,000 patients are affected in the UK. Its incidence has been rising, and while in earlier decades it was mostly a disease of the Western world, its incidence and prevalence is picking up throughout the world including China. It is a substantial health care issue.
This work is licensed under a Creative Commons Licence. If you use this content on your site please link back to this page.